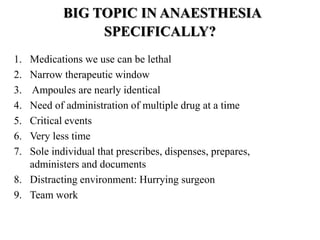
World Anesthesia Day aims to improve medication safety by sharing best practices on social media. Medication errors are a leading cause of avoidable patient harm and cost $42 billion annually. Anesthesiologists are leaders in medication safety due to the high-risk nature of the drugs administered. Key strategies to reduce errors include standardized packaging, pre-preparing syringes, double checks, and promoting a culture of reporting errors to address systemic issues.