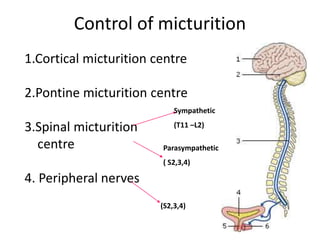
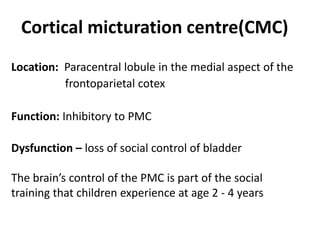
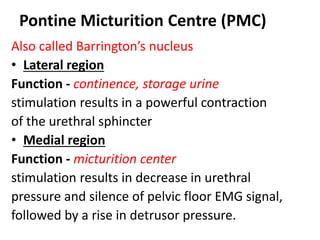
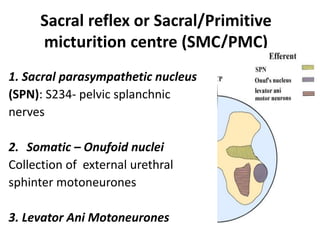
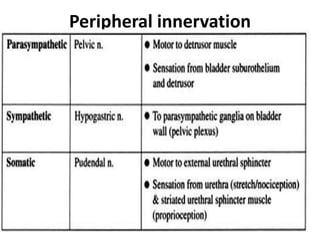
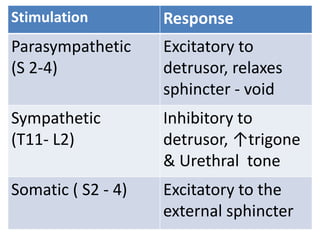
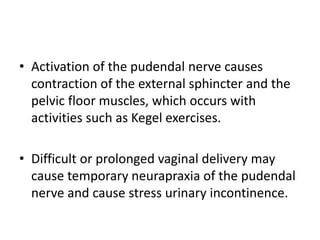
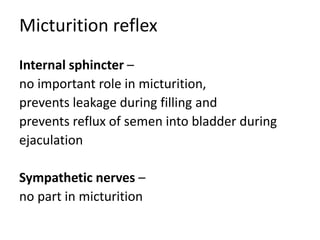
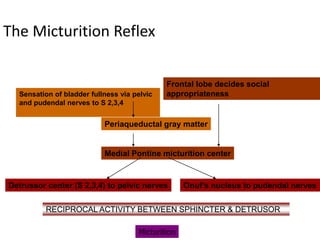
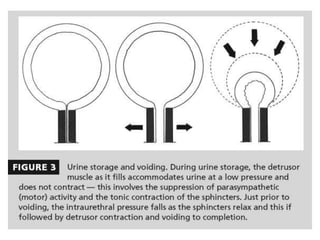
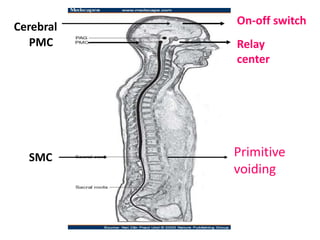
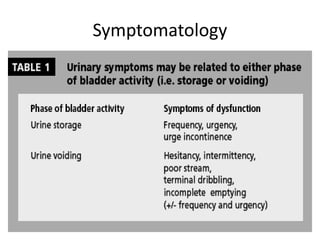
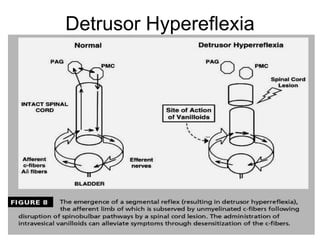
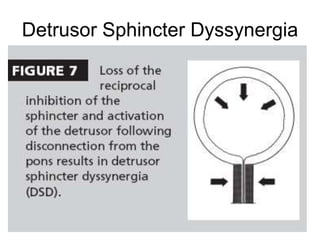
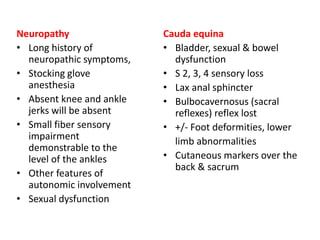
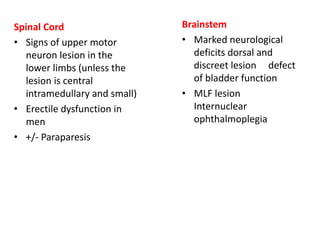
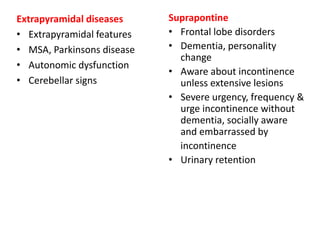
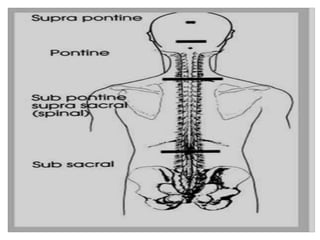
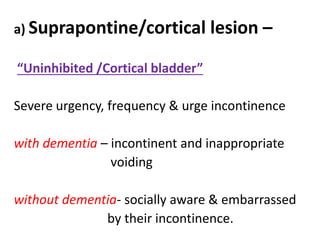
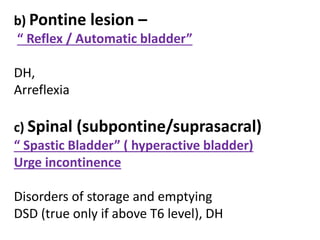
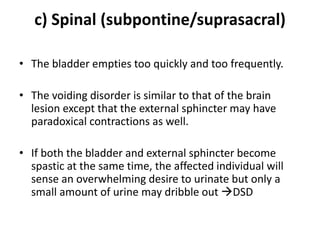
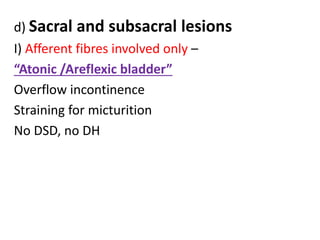
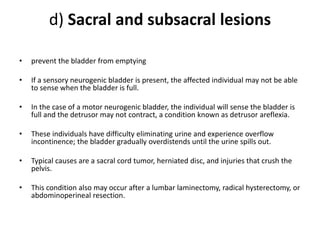
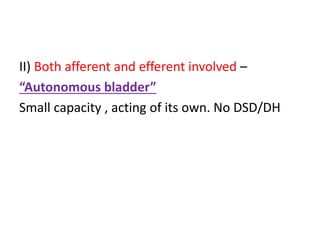
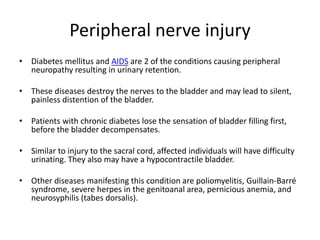
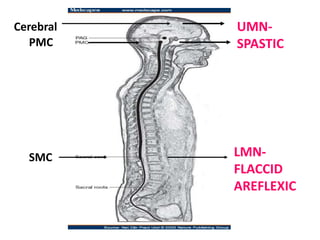
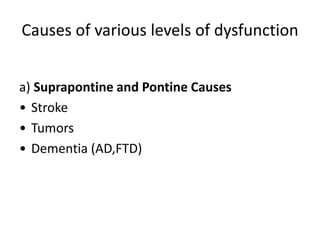
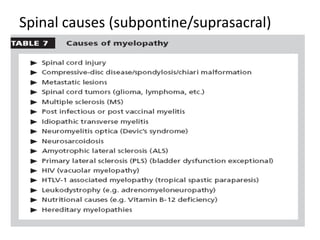
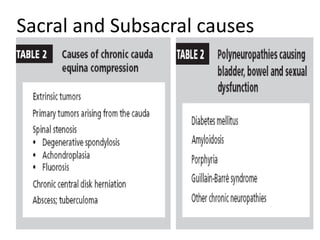
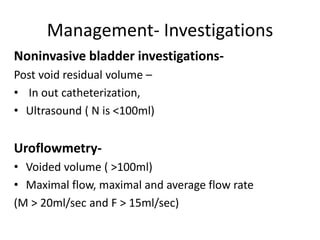
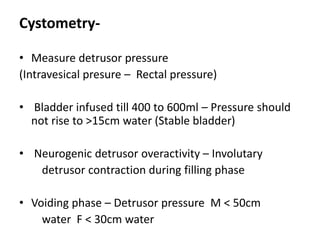
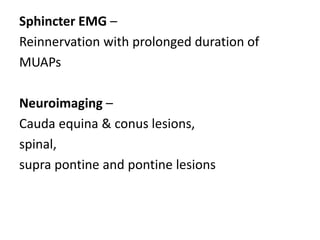
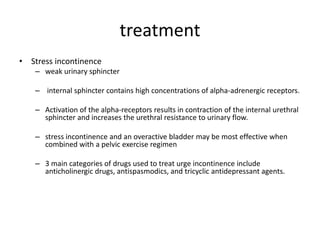
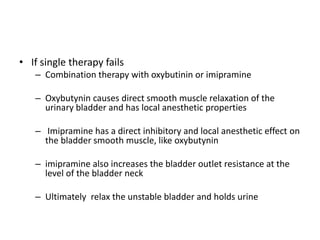
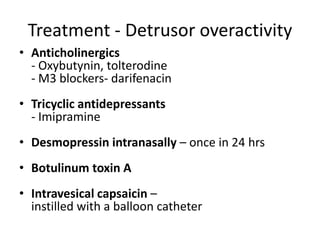
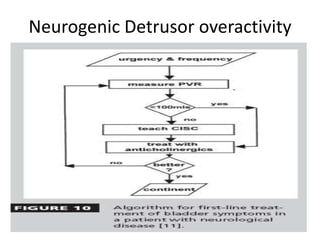
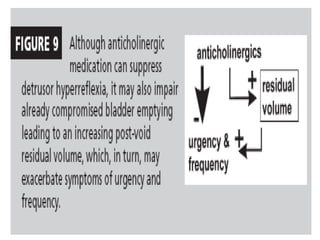
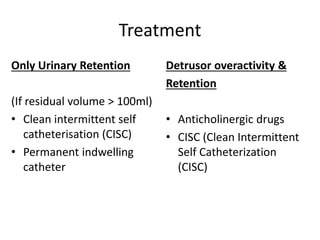
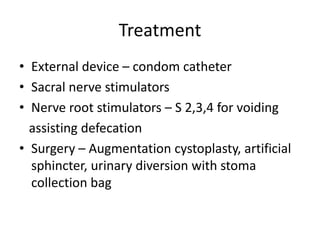
This document discusses neurogenic bladder and its management. It begins by outlining the physiology of normal bladder control and describes various types of neurogenic bladder dysfunction that can occur depending on the level of spinal cord or brain injury, including detrusor hyperreflexia, detrusor sphincter dyssynergia, and detrusor areflexia. Diagnostic investigations and treatments are then discussed, including medications, catheterization, neuromodulation, and surgeries. The goal of treatment is to balance bladder emptying and continence for each type of neurogenic bladder dysfunction.