- 130 million infants are born each year, 10% require resuscitation and 3% develop birth asphyxia requiring resuscitation, with 900,000 dying each year. Resuscitation is more often needed for preterm infants.
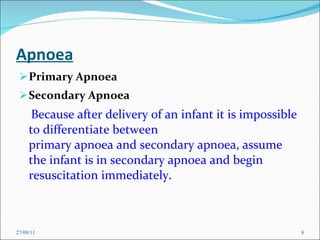
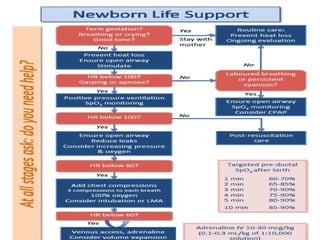
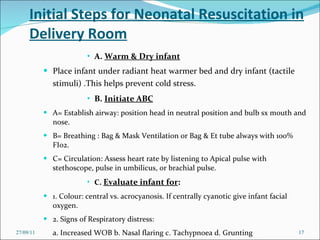
- The goals of resuscitation are to minimize heat loss, establish normal breathing and lung function, increase oxygen levels, and support adequate blood circulation.
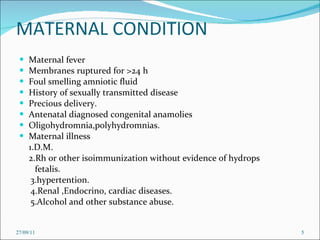
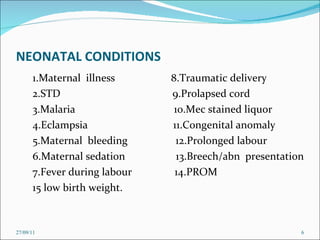
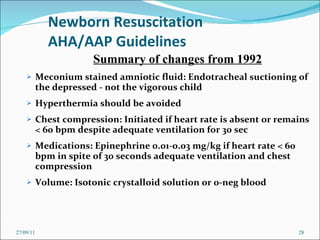
- Risk factors for needing resuscitation include maternal infections, illnesses, trauma during delivery, and fetal conditions like meconium in the amniotic fluid or congenital anomalies.