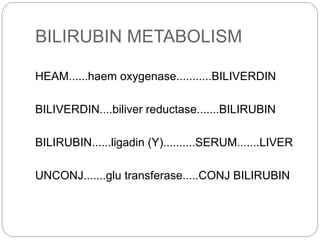
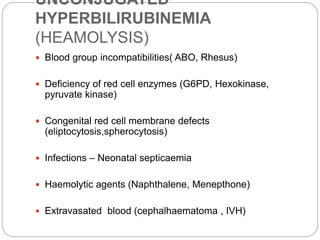
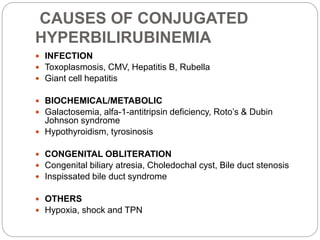
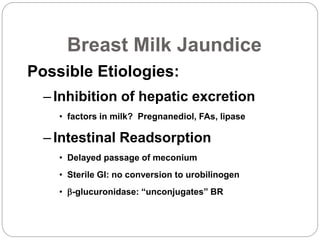
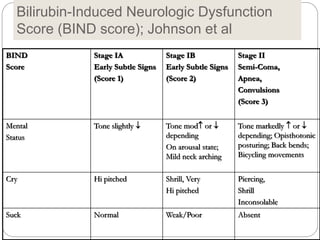
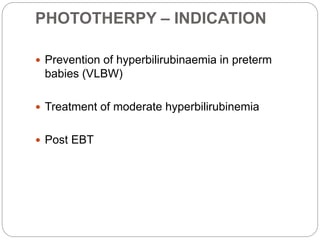
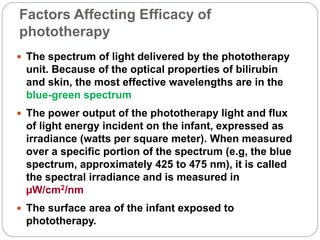
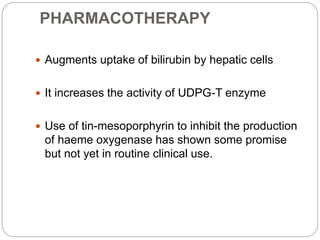
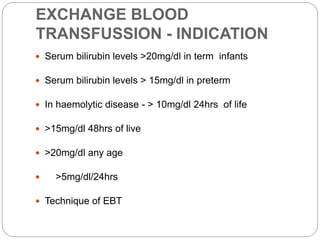
This document discusses neonatal jaundice, including its definition, etiology, bilirubin production and metabolism, types of hyperbilirubinemia, causes, clinical features, kernicterus, and treatment options. Neonatal jaundice is caused by increased bilirubin levels and results in a yellowish skin and eye discoloration. Bilirubin is produced from the breakdown of hemoglobin. Treatment depends on the type and severity of hyperbilirubinemia, and may include phototherapy, exchange blood transfusions, or medications to increase bilirubin clearance from the liver.