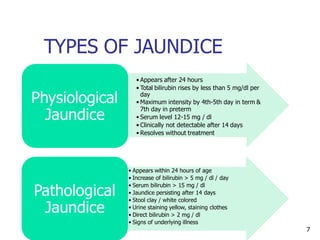
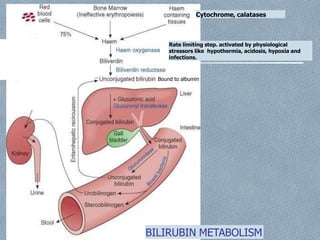
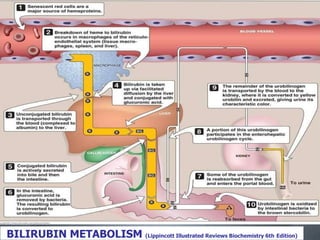
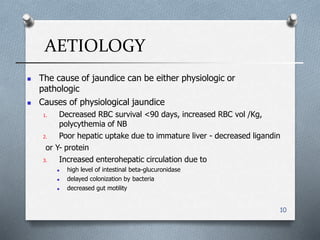
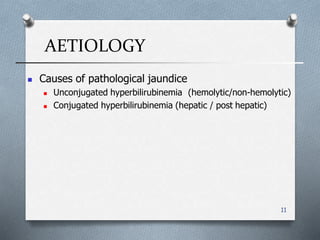
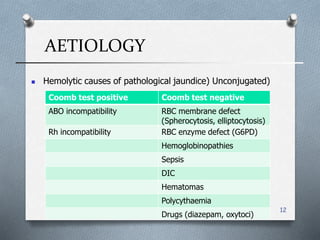
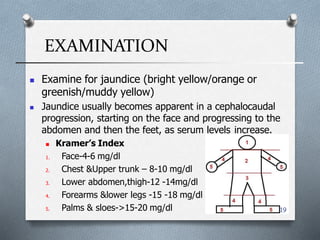
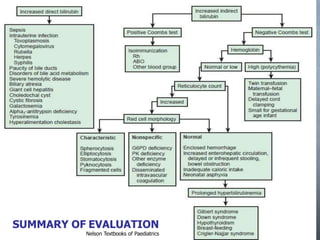
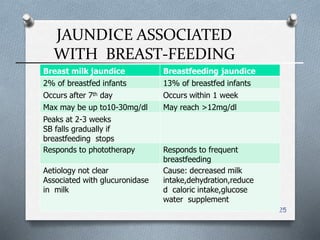
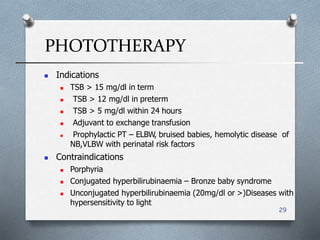
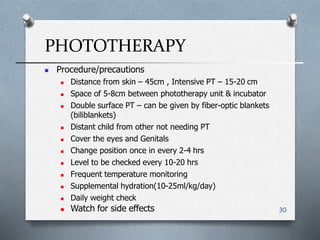
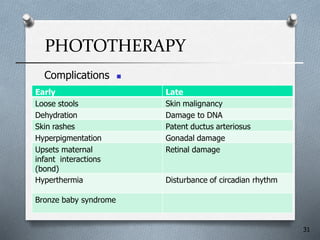
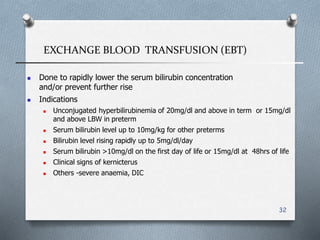
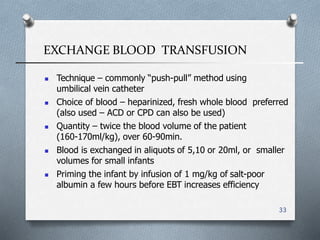
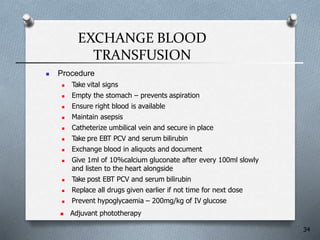
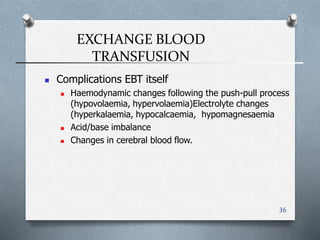
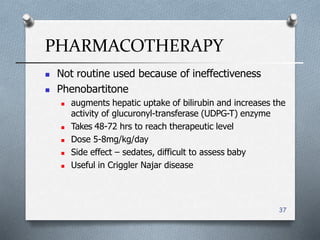
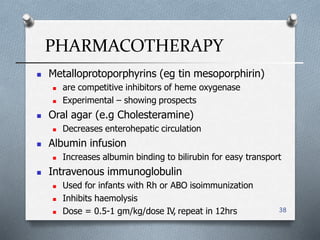
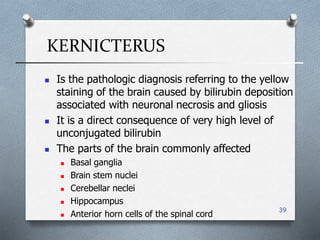
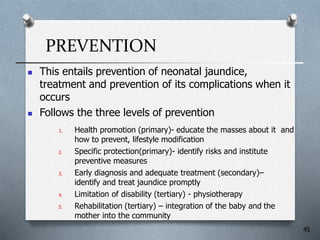
This document provides an outline and overview of neonatal jaundice. It discusses the epidemiology, bilirubin metabolism, causes (physiological and pathological), clinical presentation, management including phototherapy and exchange blood transfusion, complications and prevention of neonatal jaundice. Neonatal jaundice is a common condition seen in newborns due to elevated bilirubin levels that can cause yellowing of the skin if not properly managed.