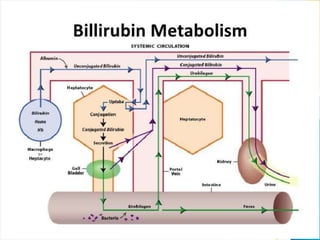
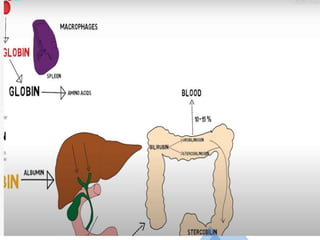
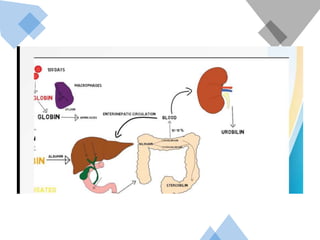
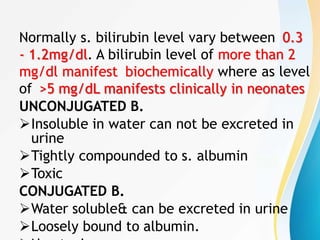
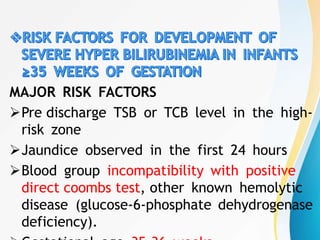
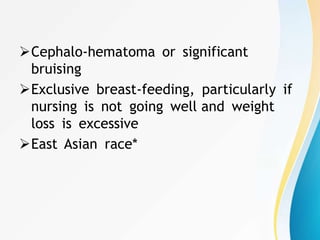
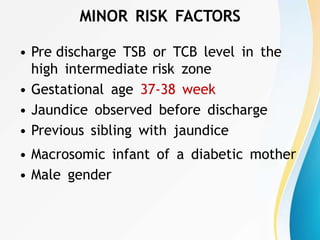
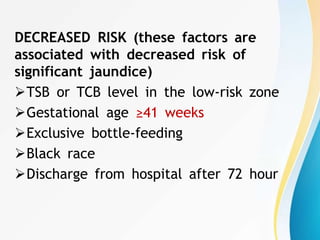
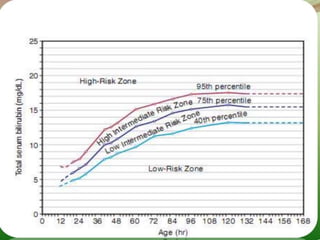
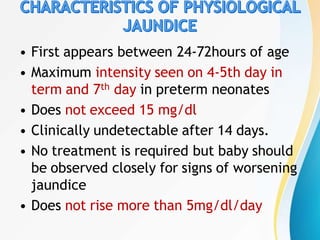
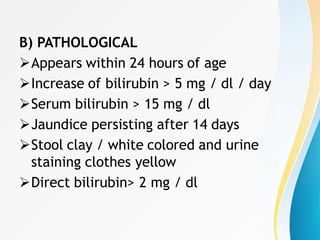
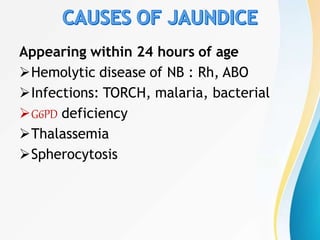
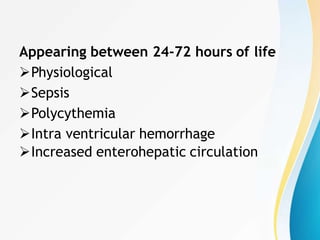
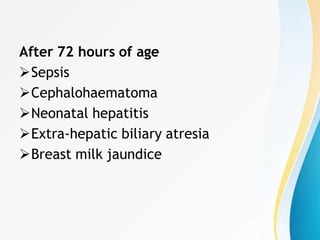
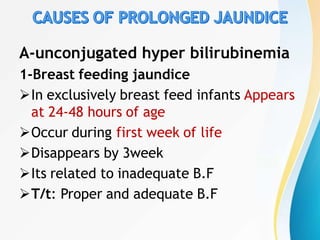
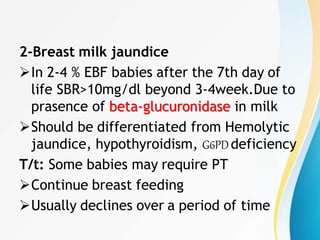
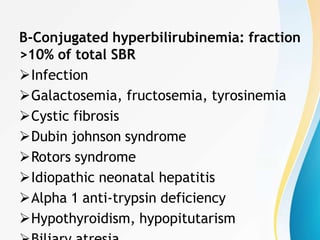
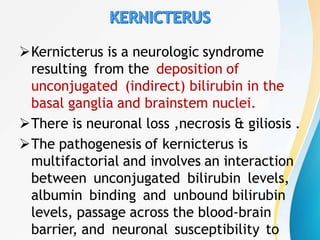
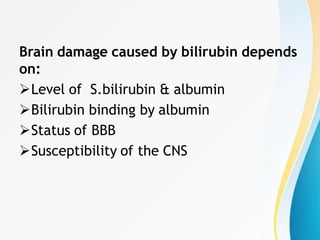
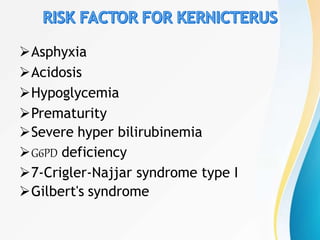
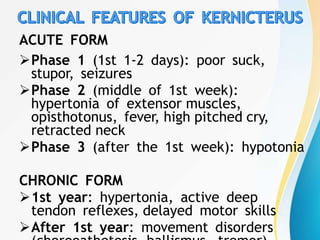
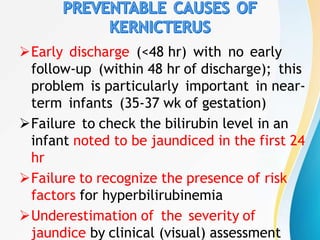
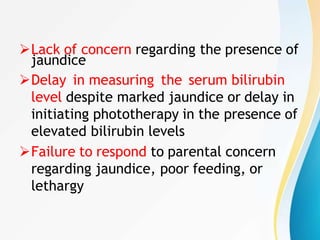
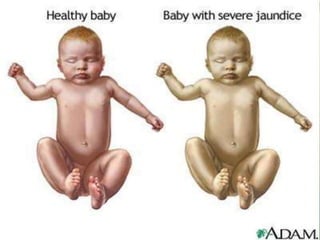
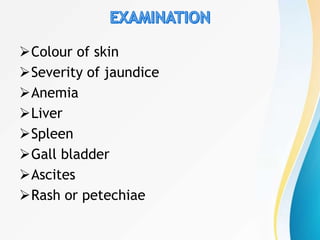
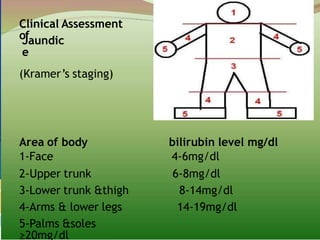
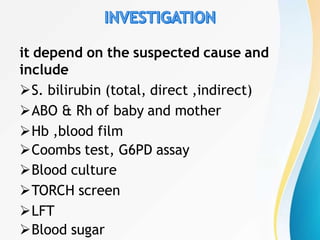
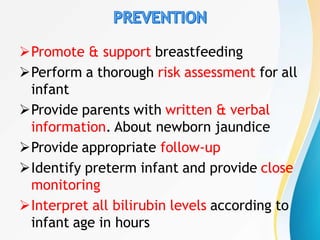
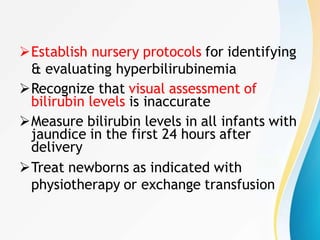
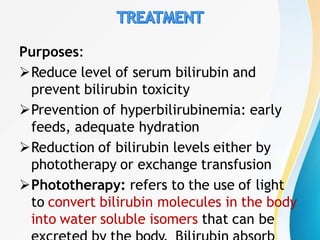
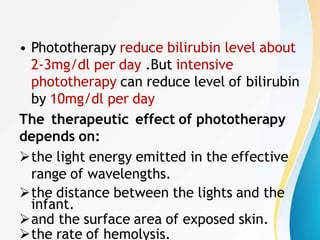
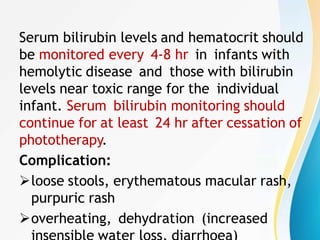
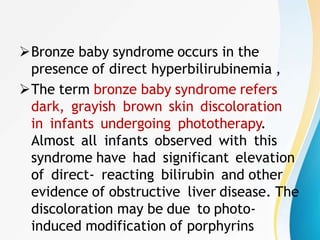
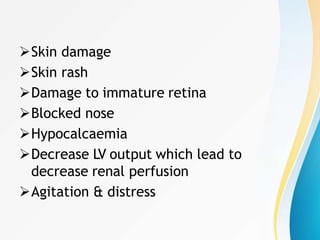
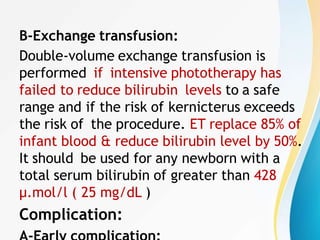
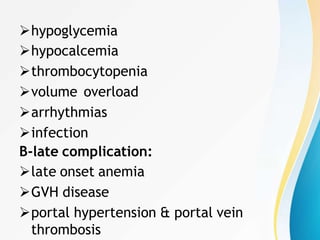
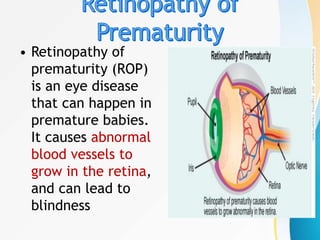
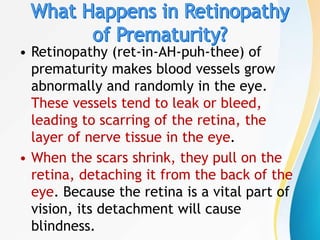
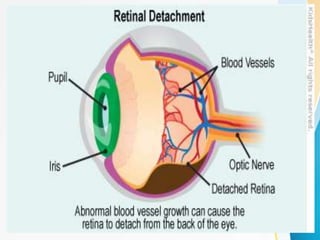
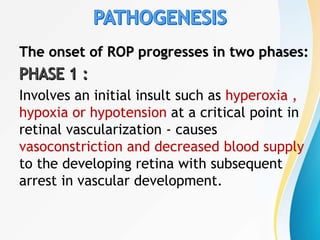
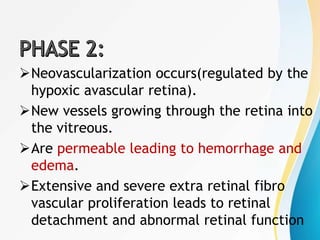
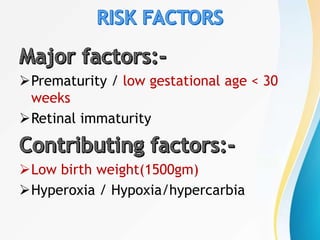
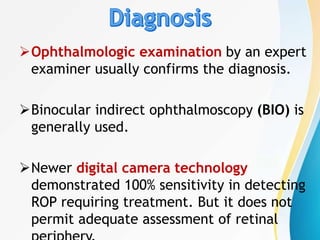
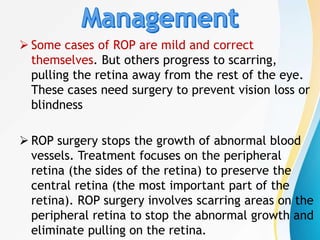
This document provides information about neonatal jaundice and retinopathy of prematurity (ROP). It defines these conditions and discusses their risk factors, etiology, types, diagnostic evaluation, and management. For neonatal jaundice, the document covers bilirubin metabolism, risk factors, types of jaundice, evaluation, complications like kernicterus, and treatment methods like phototherapy and exchange transfusion. For ROP, it describes the abnormal blood vessel growth in the retina that can lead to blindness if left untreated.