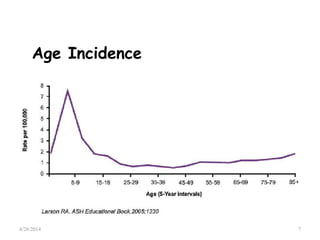
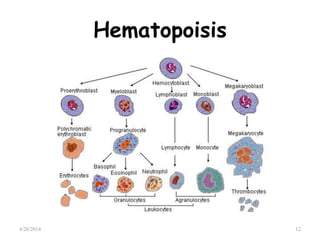
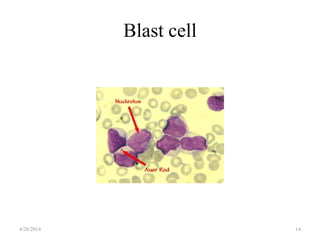
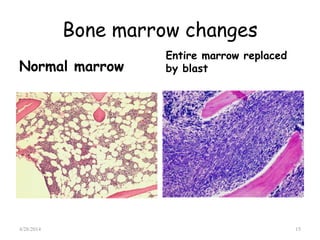
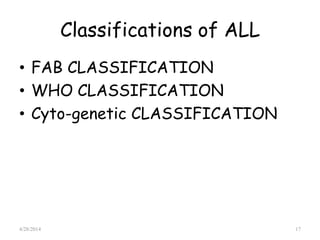
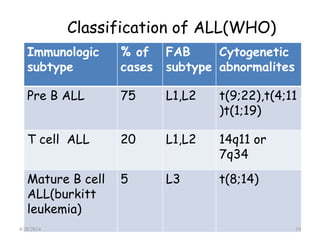
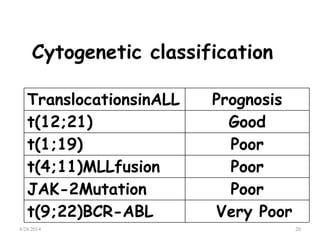
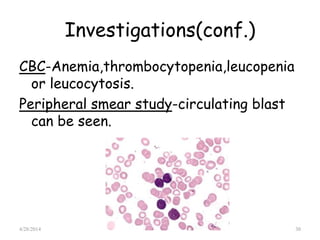
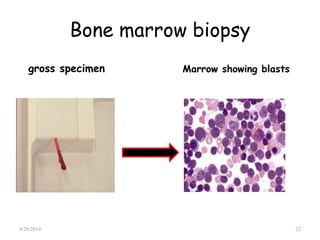
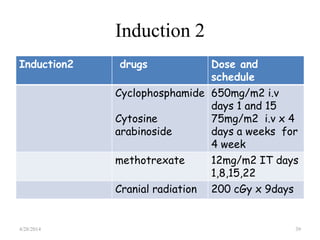
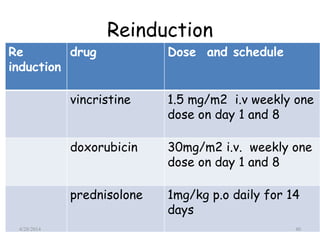
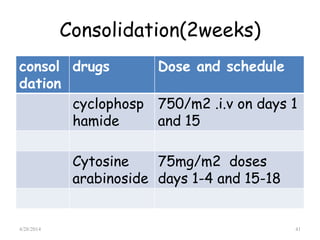
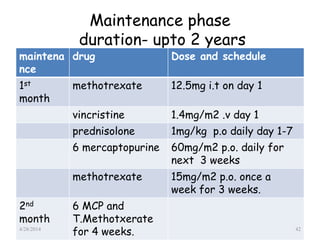
This document provides an overview of acute lymphoblastic leukemia (ALL) in children, including its definition, classification, epidemiology, pathophysiology, diagnosis, and treatment. It discusses how ALL results from mutations that cause immature white blood cells to crowd out the bone marrow. The diagnosis involves blood tests and bone marrow biopsies showing an excess of lymphoblasts. Treatment typically involves chemotherapy in multiple phases over 2 years, including induction, consolidation, and maintenance. Newer targeted drugs and stem cell transplants are used in high-risk cases. Prognostic factors like age, white blood cell count, and specific genetic abnormalities determine treatment approach and predicted outcomes.