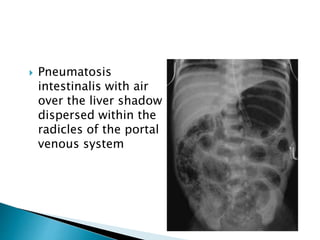
This document discusses several surgical emergencies that can occur in neonates, including intestinal obstruction, necrotizing enterocolitis, and intussusception. It provides details on the causes, signs, symptoms, diagnostic approaches and treatment options for these conditions. Key points covered include the risk factors for necrotizing enterocolitis, its clinical stages and management involving initial medical therapy or later potential surgery. Diagnostic tools like abdominal x-rays and contrast enemas are also outlined.