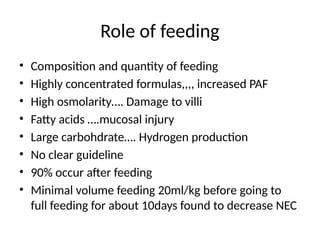
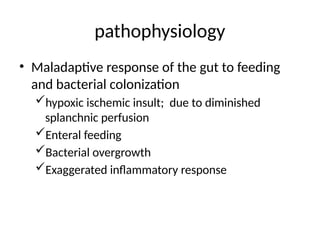
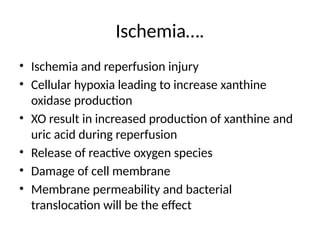
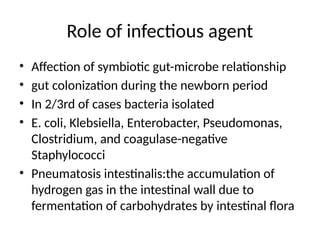
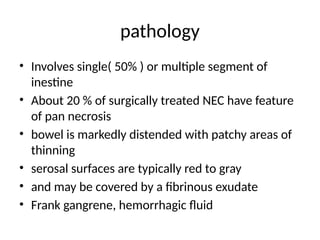
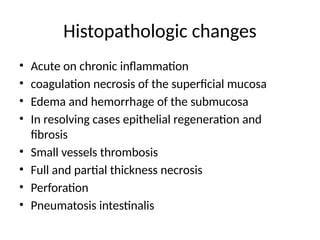
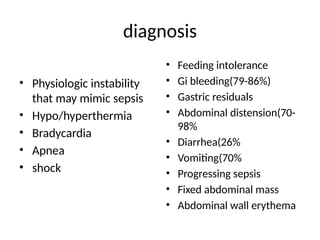
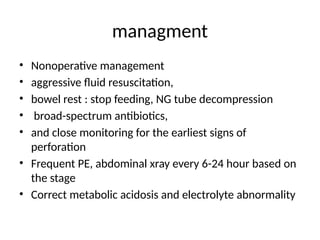
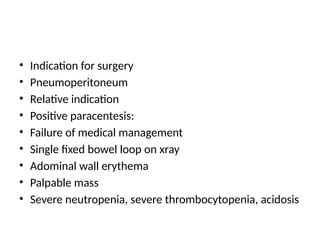
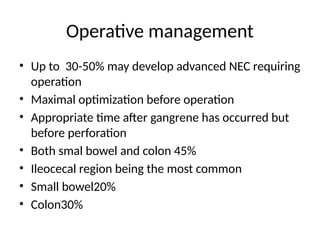
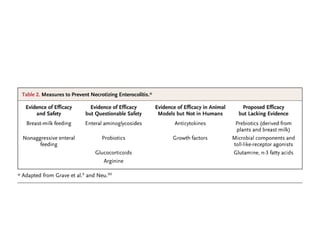
Necrotizing enterocolitis (NEC) is an inflammatory condition of the gastrointestinal tract primarily affecting preterm infants, characterized by high mortality and morbidity rates in the neonatal intensive care unit (NICU). Diagnosis and treatment remain challenging, with feeding practices, gut colonization, and ischemic injury being significant contributing factors to the disease's pathophysiology. Management options include medical therapy, surgical interventions, and supportive care, with outcomes varying based on the extent of intestinal involvement and the timing of treatment.