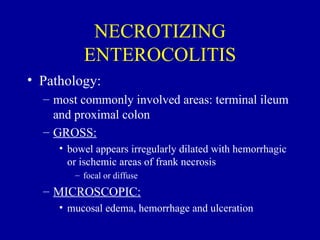
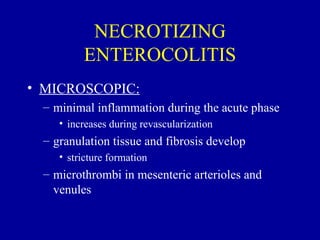
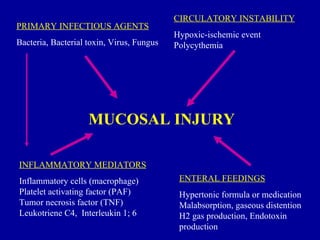
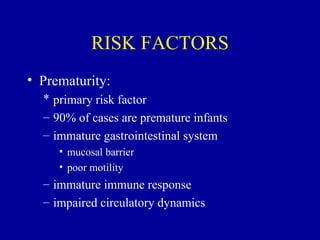
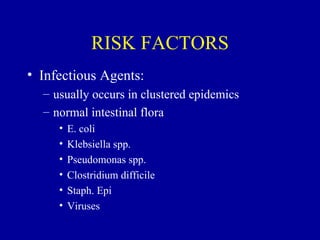
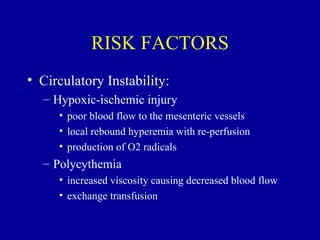
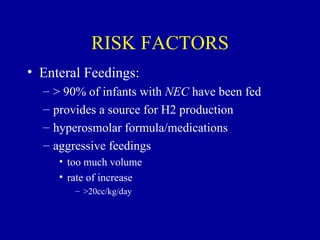
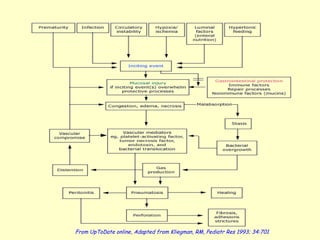
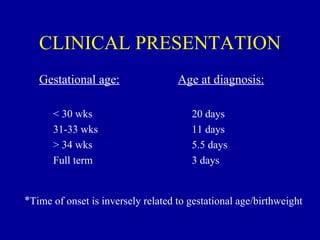
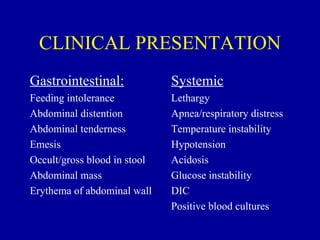
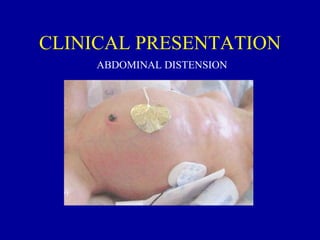
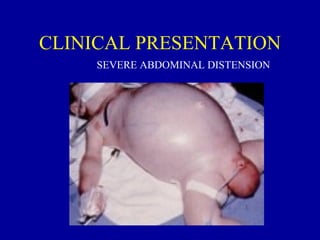
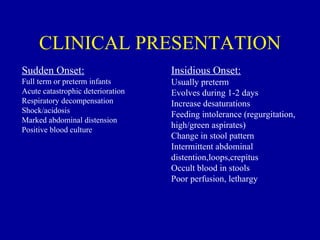
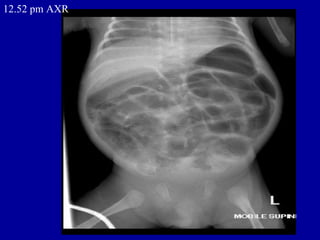
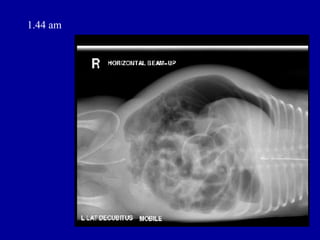
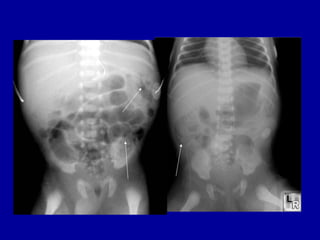
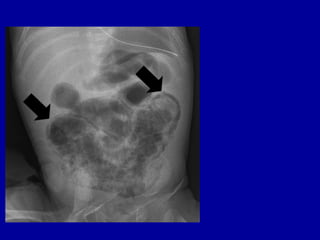
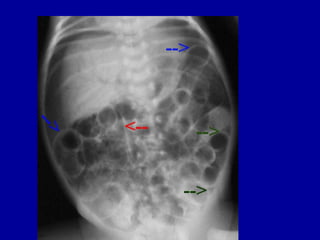
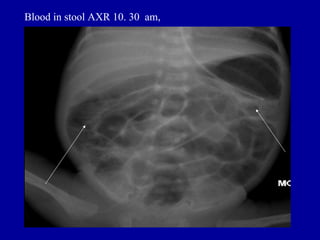
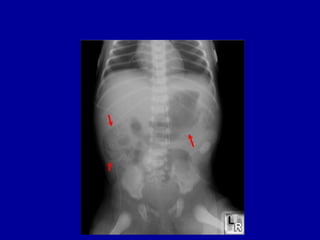
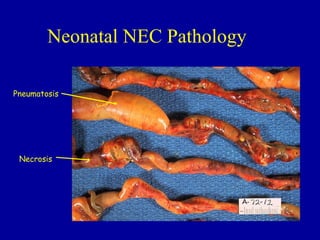
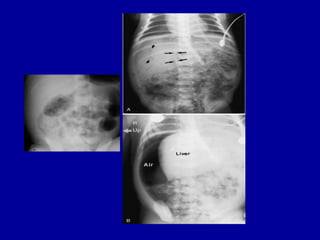
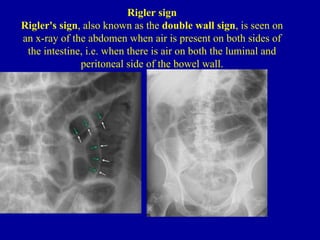
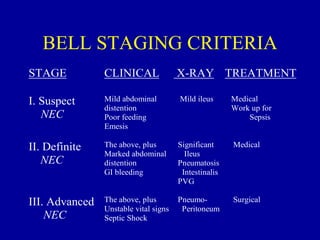
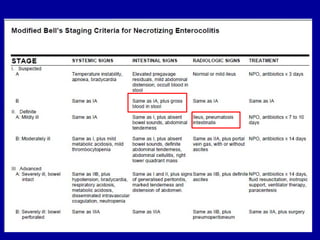
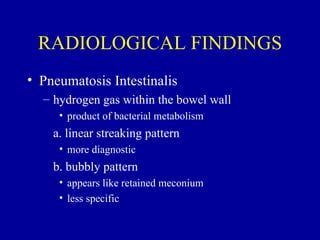
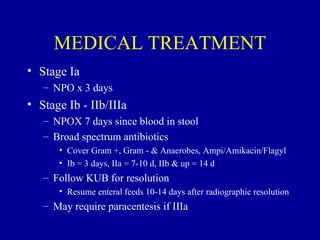
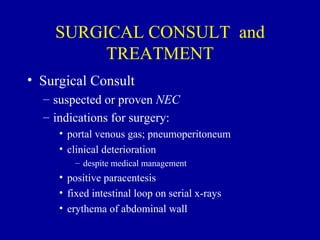
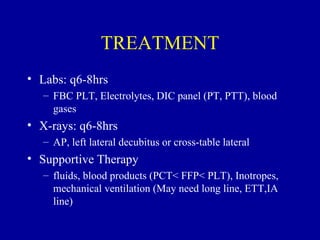
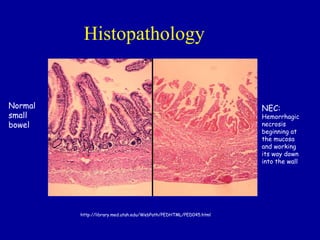
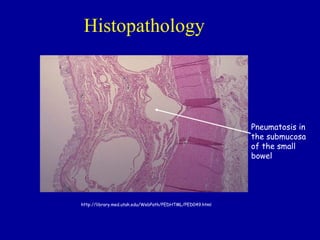
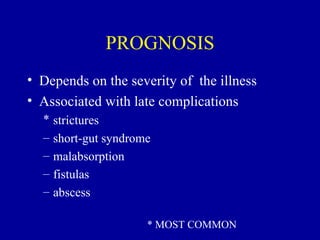
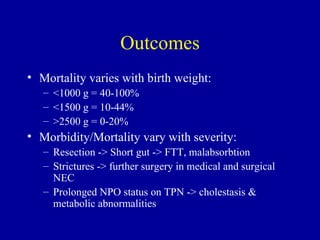
Necrotizing enterocolitis (NEC) is a leading cause of emergency surgery in neonates. It most commonly affects very low birth weight preterm infants. Classic signs on imaging include pneumatosis intestinalis, portal venous gas, and free air indicating perforation. Treatment involves management of sepsis, circulatory support, and may require surgery for advanced cases. Long-term complications are common, affecting 50% of survivors. Early diagnosis through monitoring for feeding intolerance and abdominal distension along with radiographic findings is important for optimal management of this serious gastrointestinal emergency in neonates.