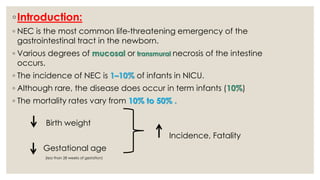
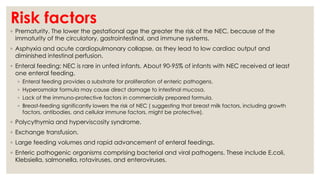
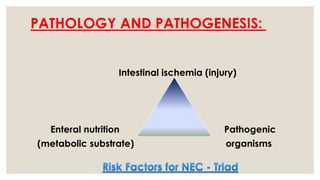
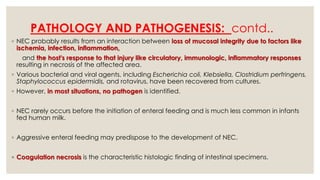
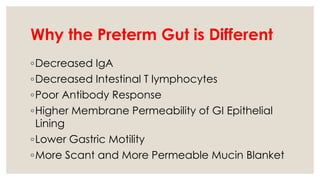
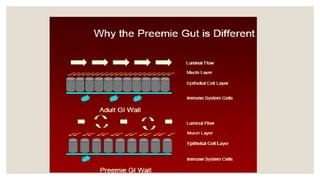
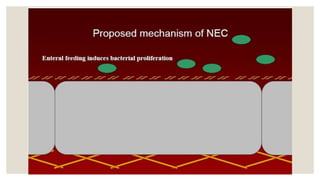
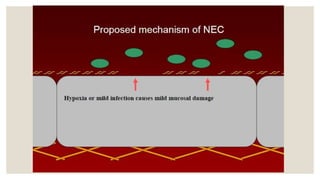
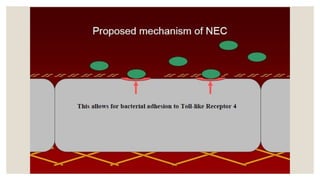
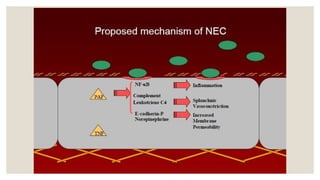
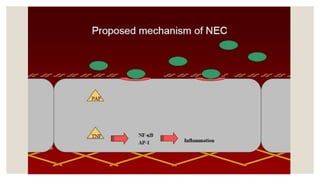
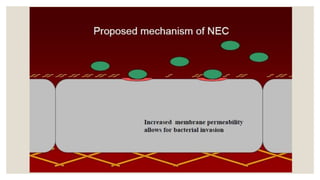
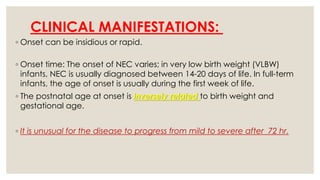
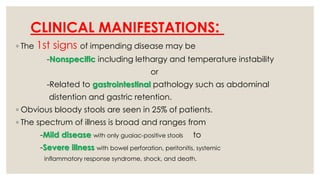
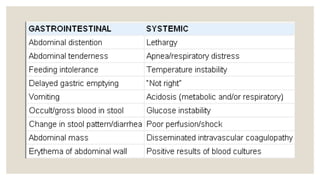
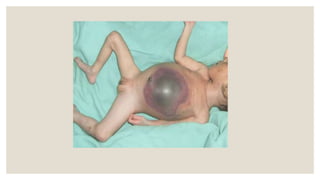
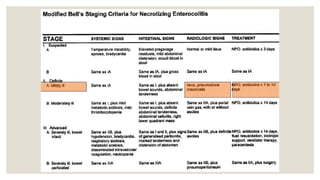
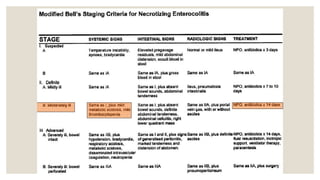
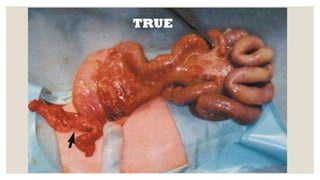
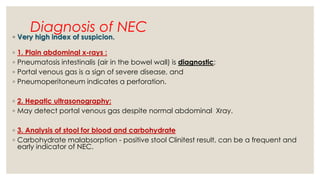
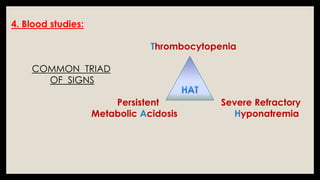
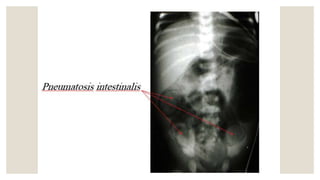
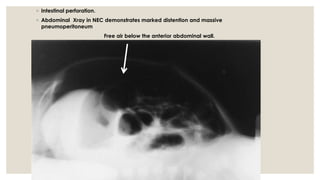
Neonatal necrotizing enterocolitis (NEC) is a serious gastrointestinal condition primarily affecting premature infants, with an incidence of 1-10% in NICU and mortality rates between 10% to 50%. Risk factors include prematurity, enteral feeding, and certain medical interventions, while early diagnosis involves radiographic evidence and clinical symptoms such as abdominal distention and bloody stools. Treatment focuses on supportive care, with surgical intervention indicated for complications like perforation, and prevention strategies include breastfeeding and careful feeding protocols.