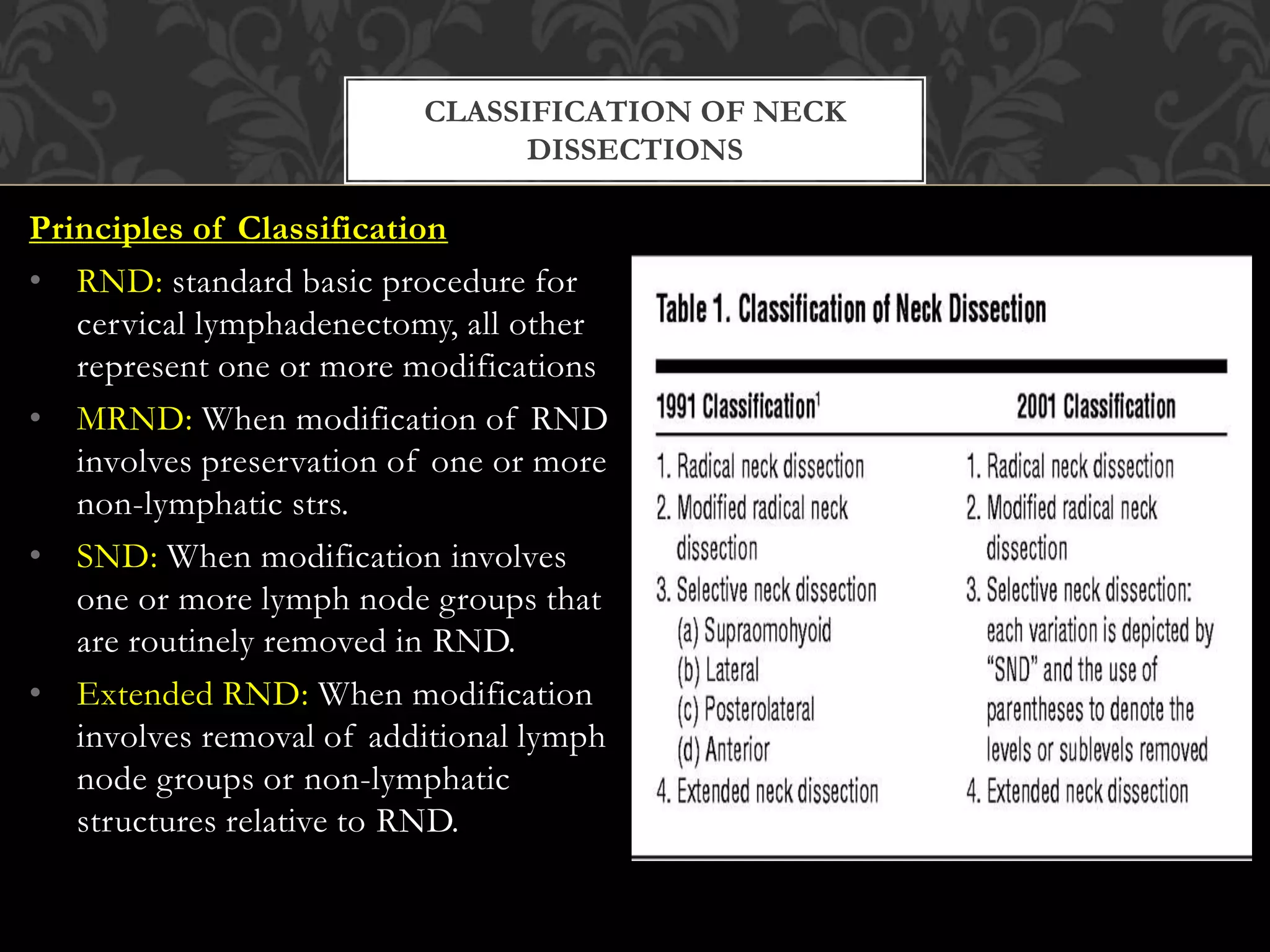
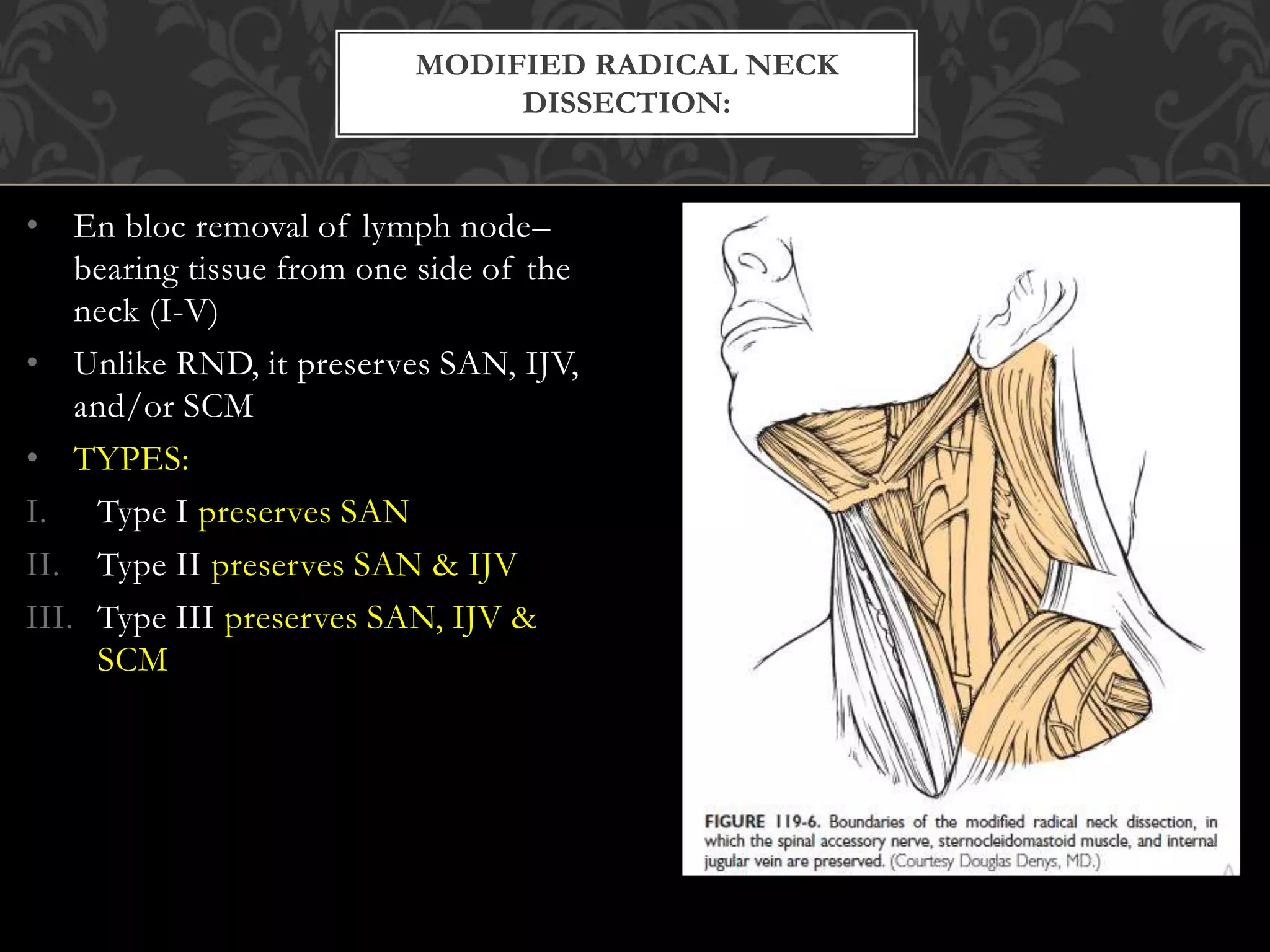
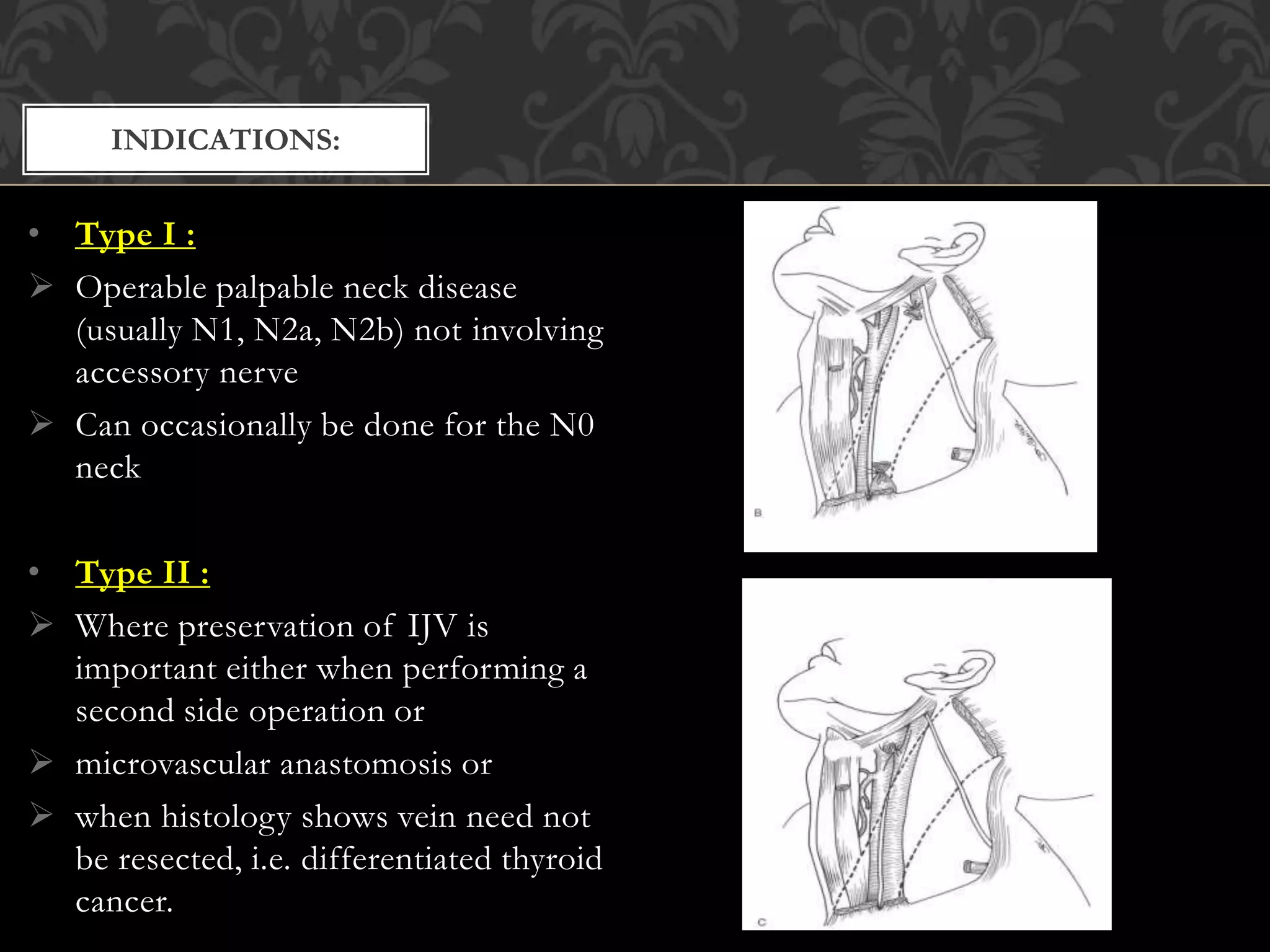
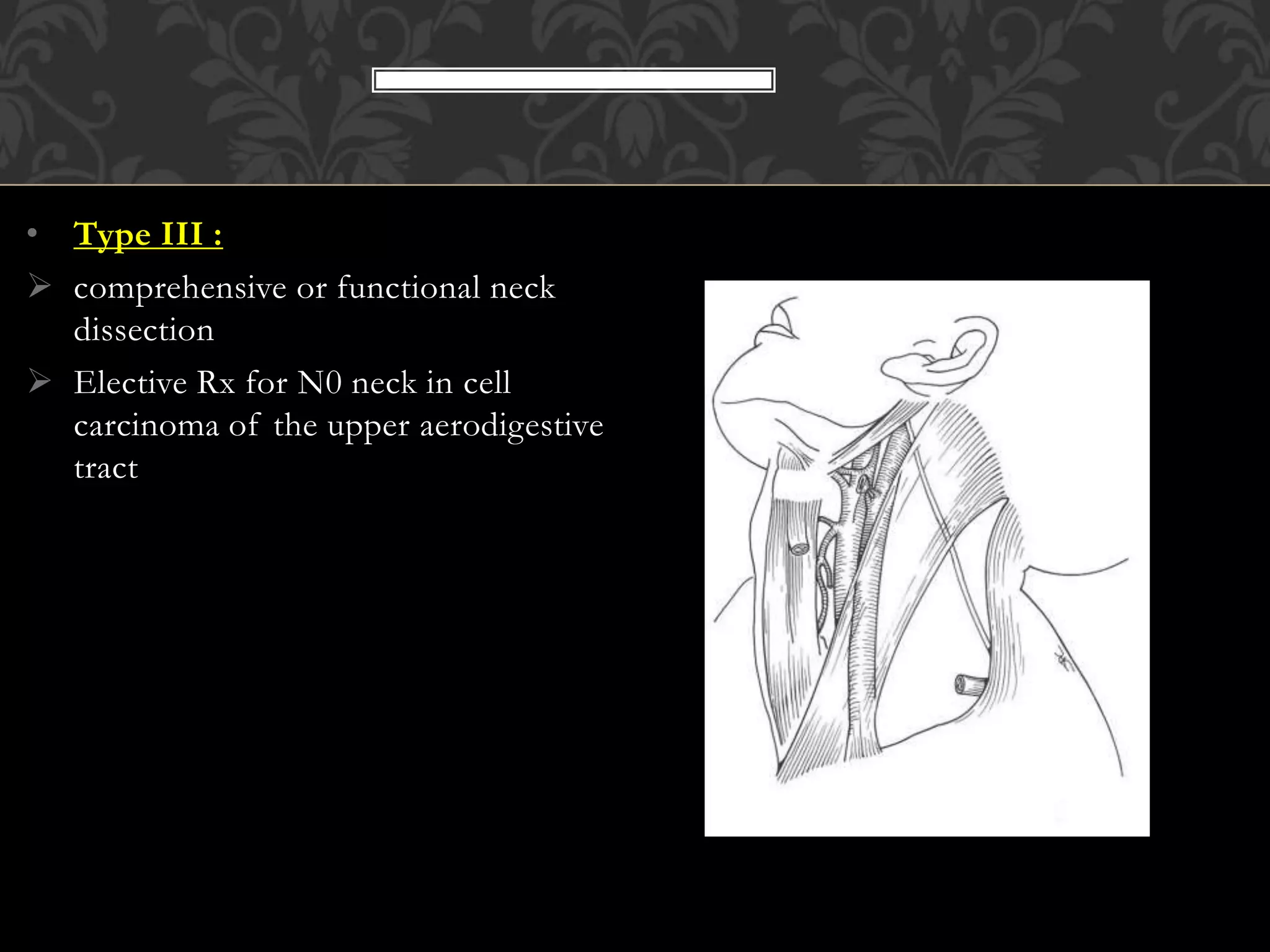
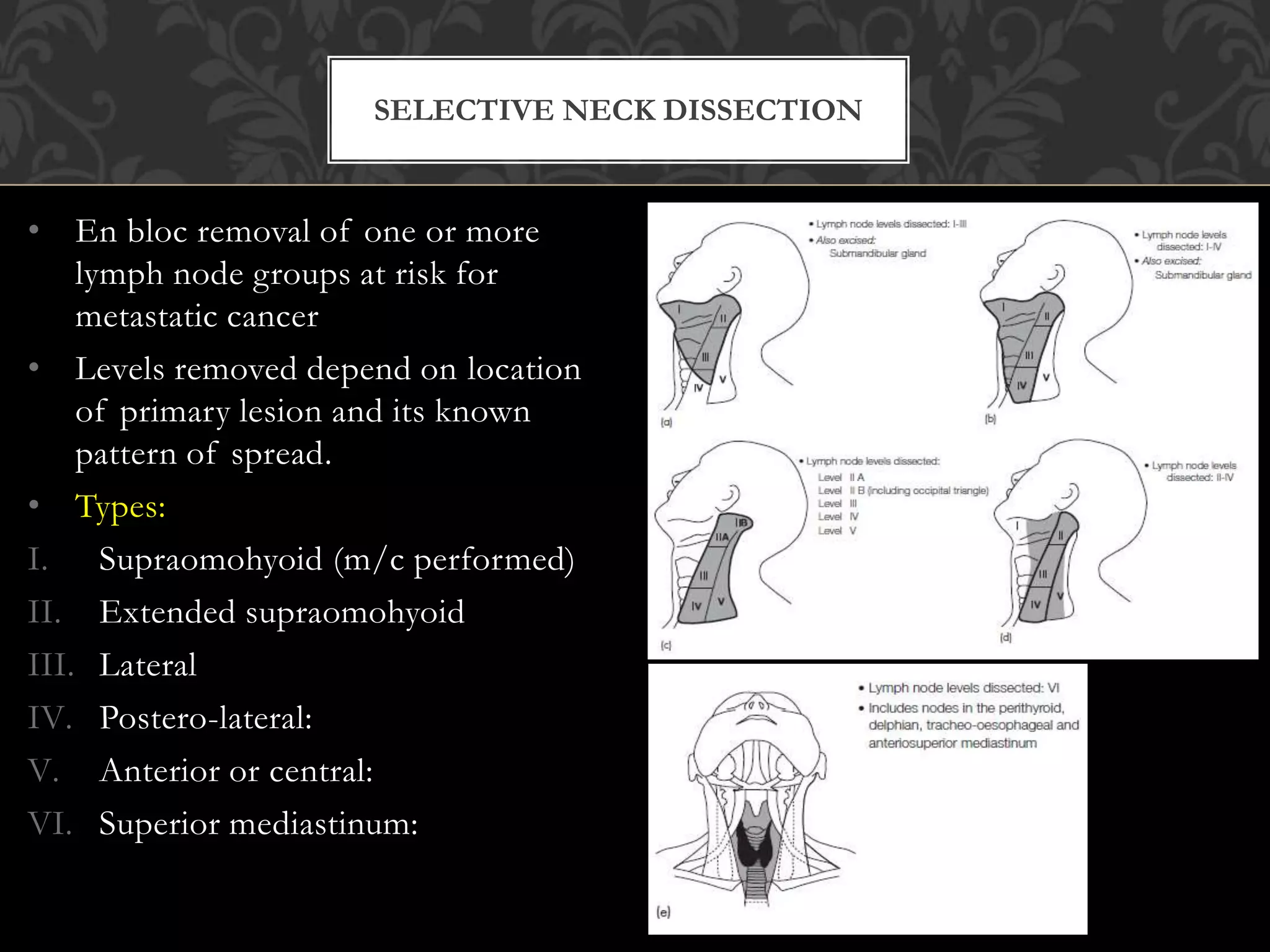
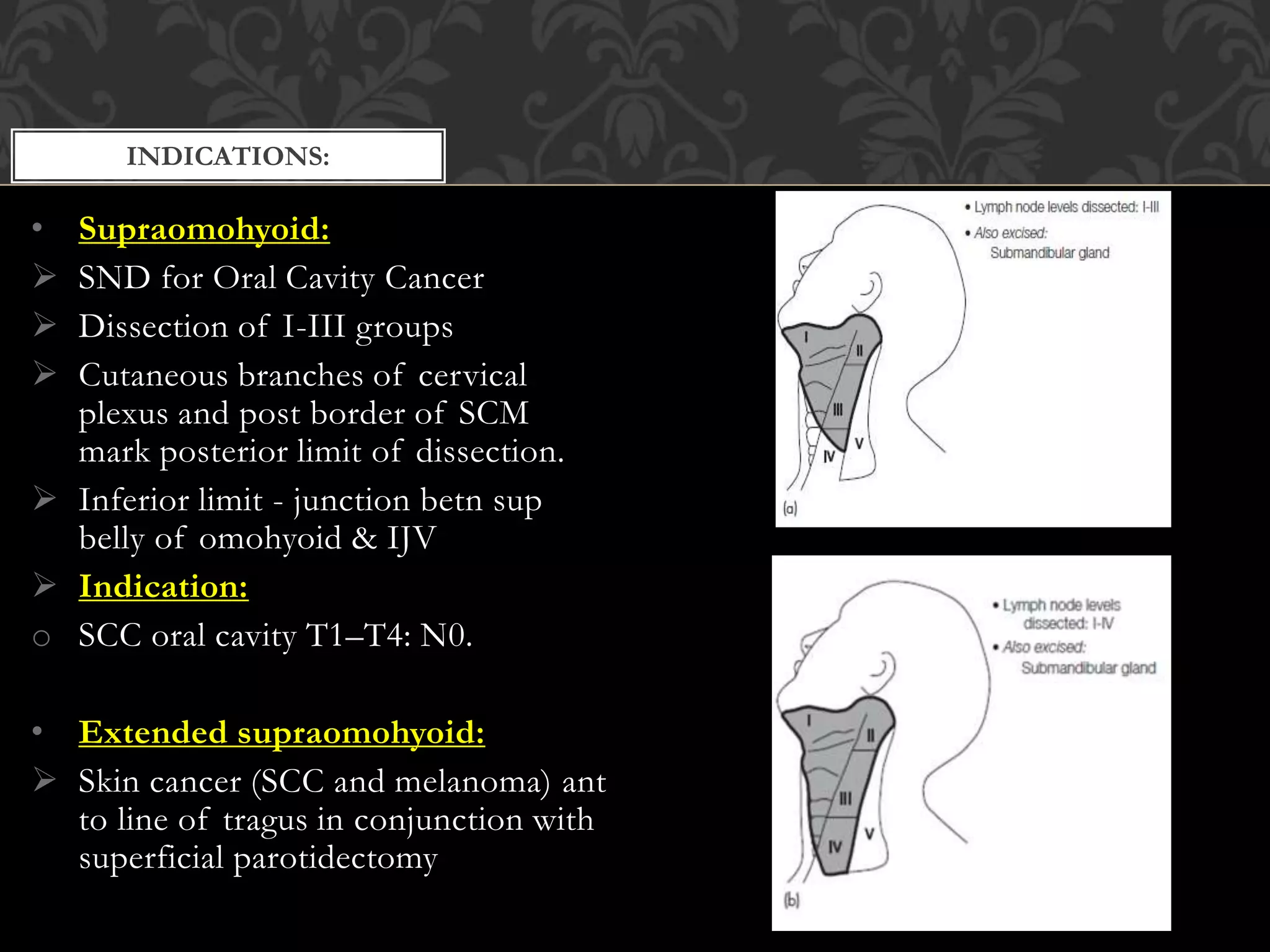
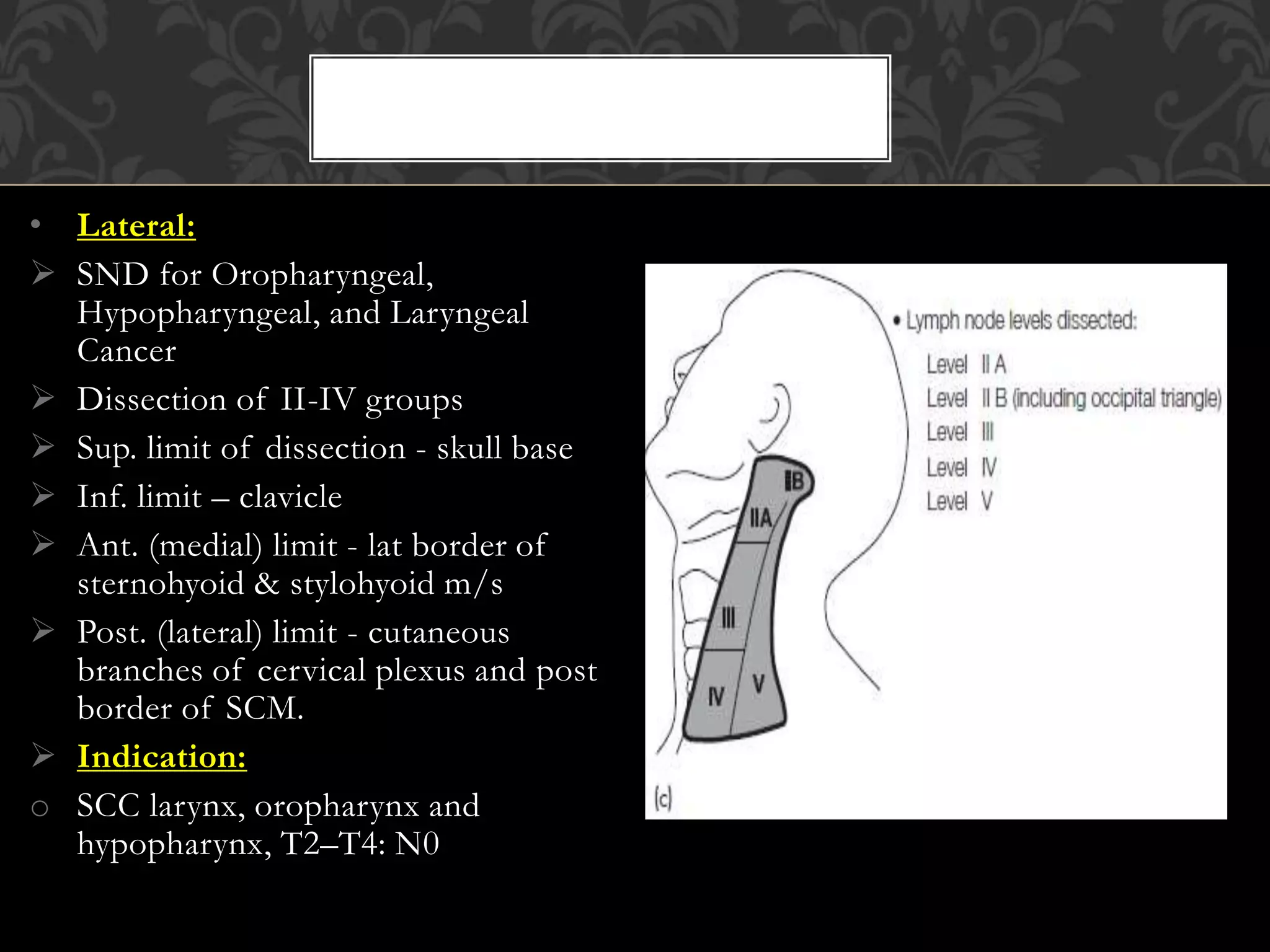
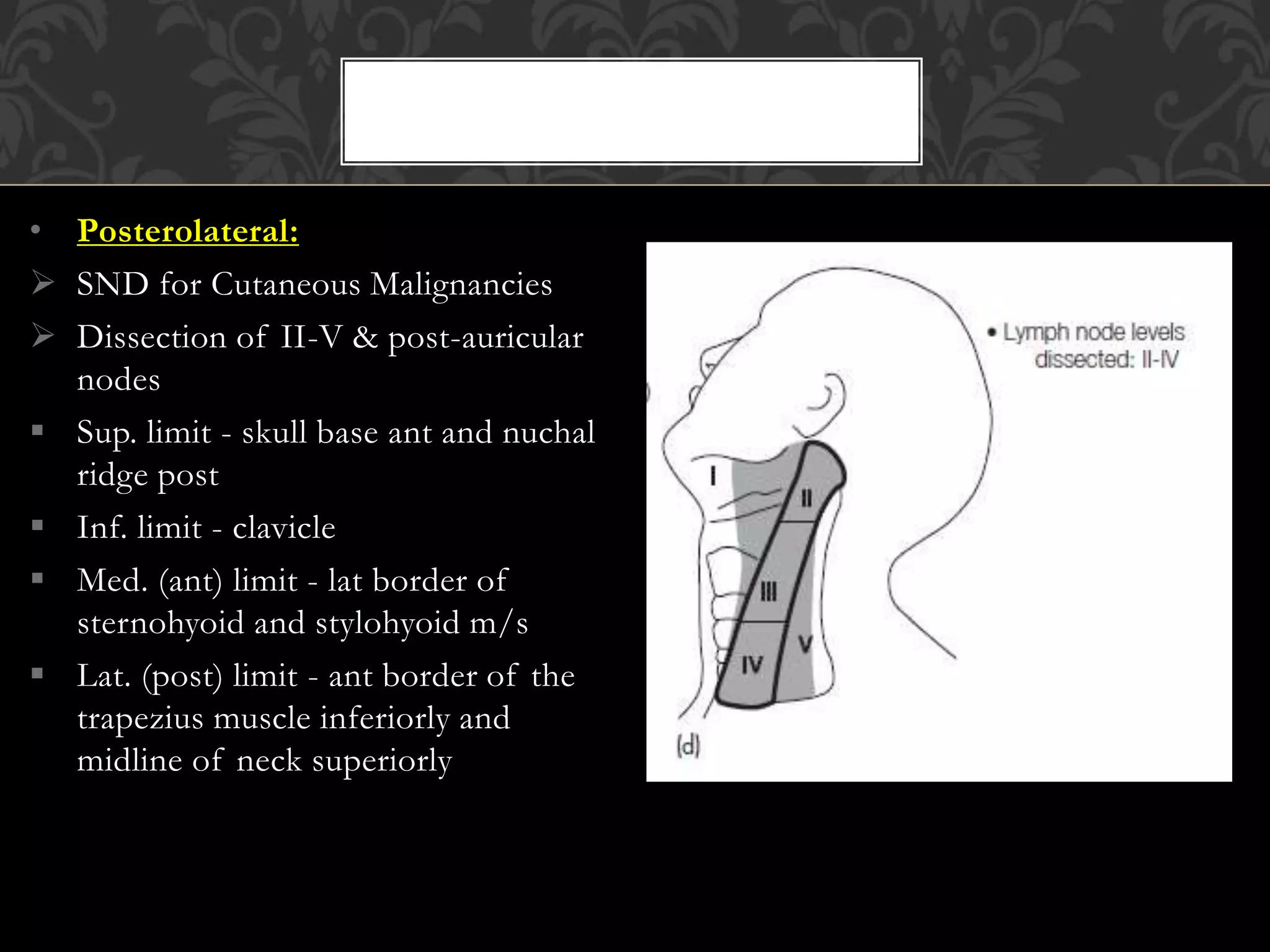
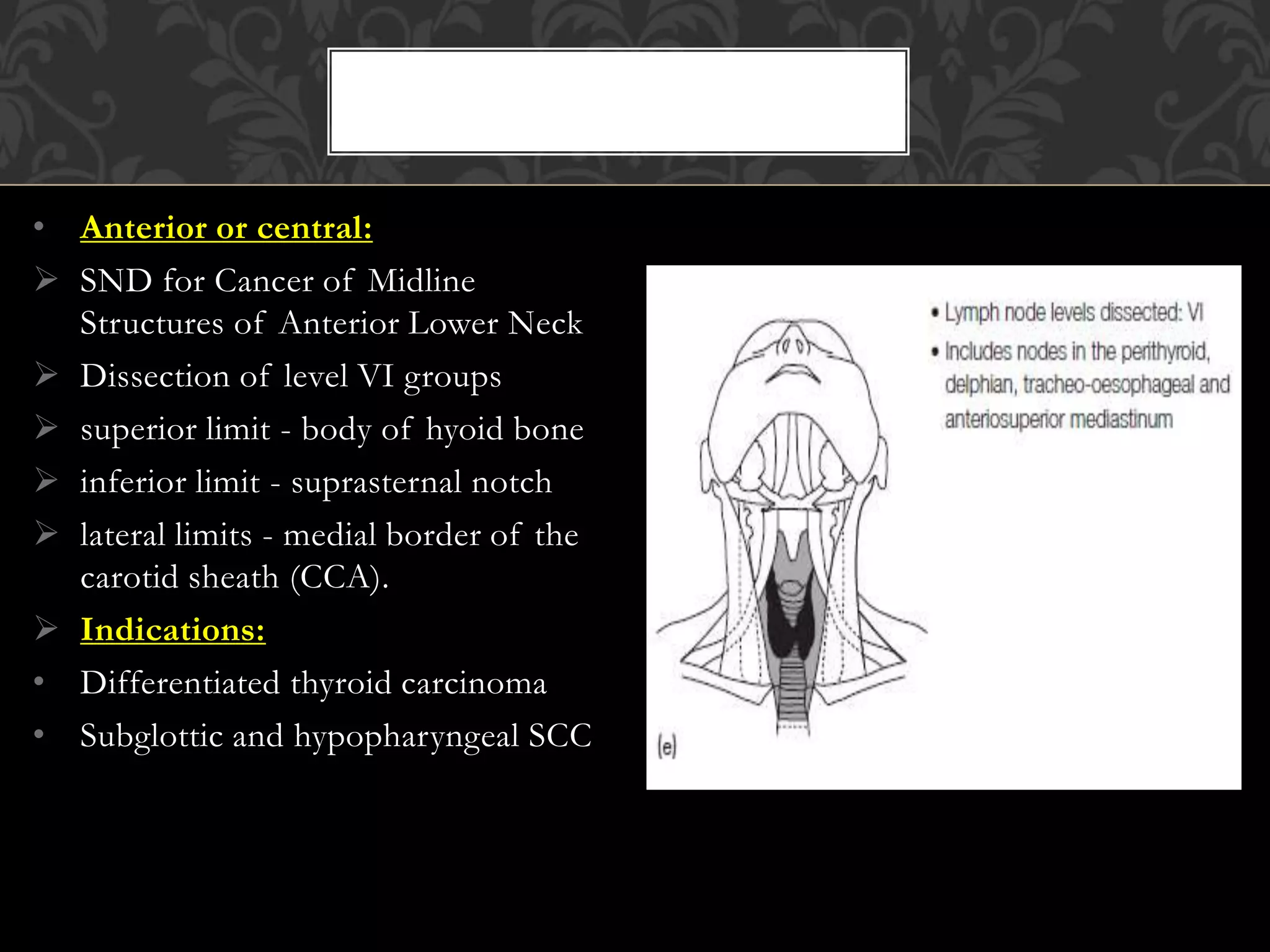
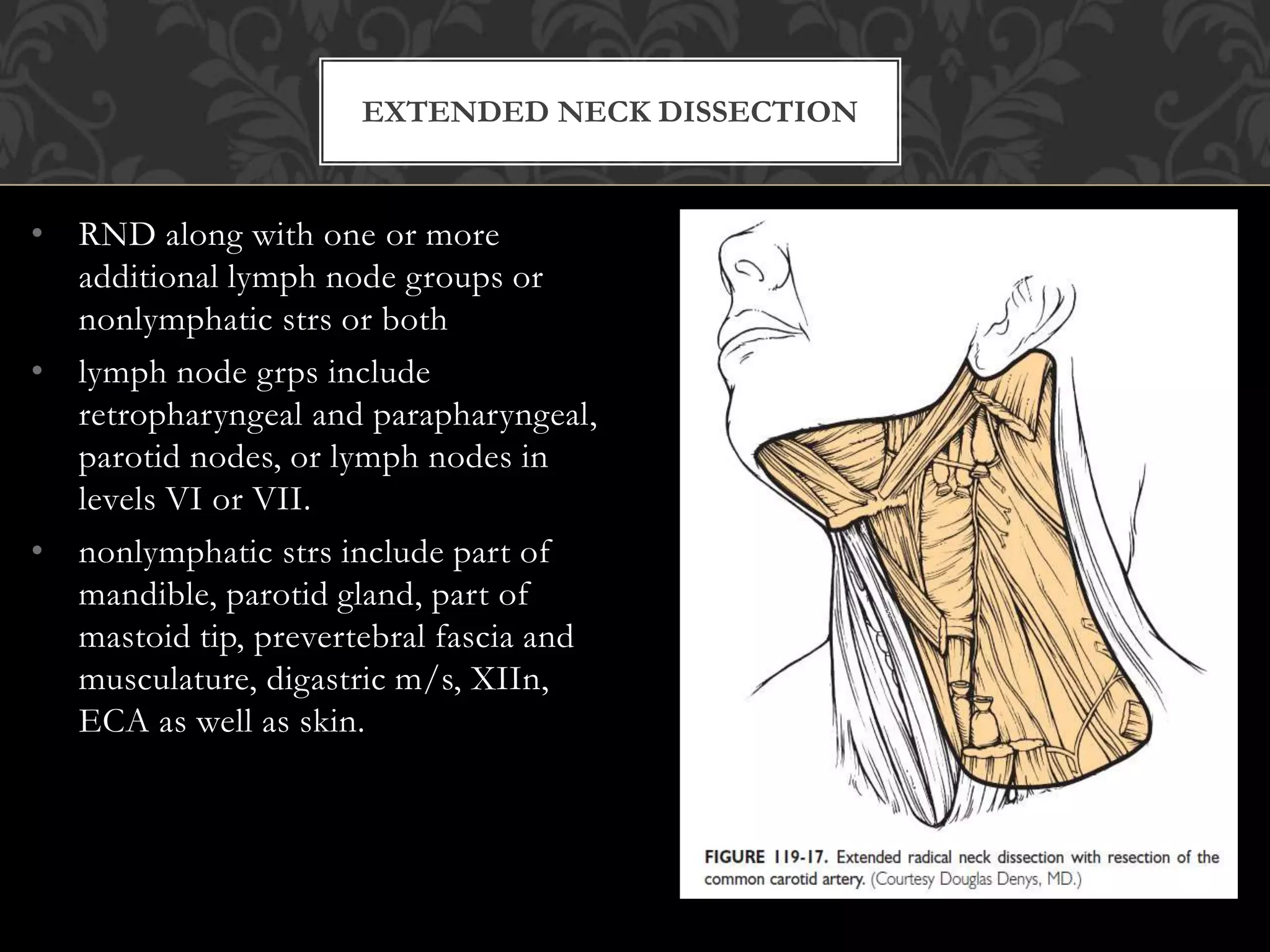
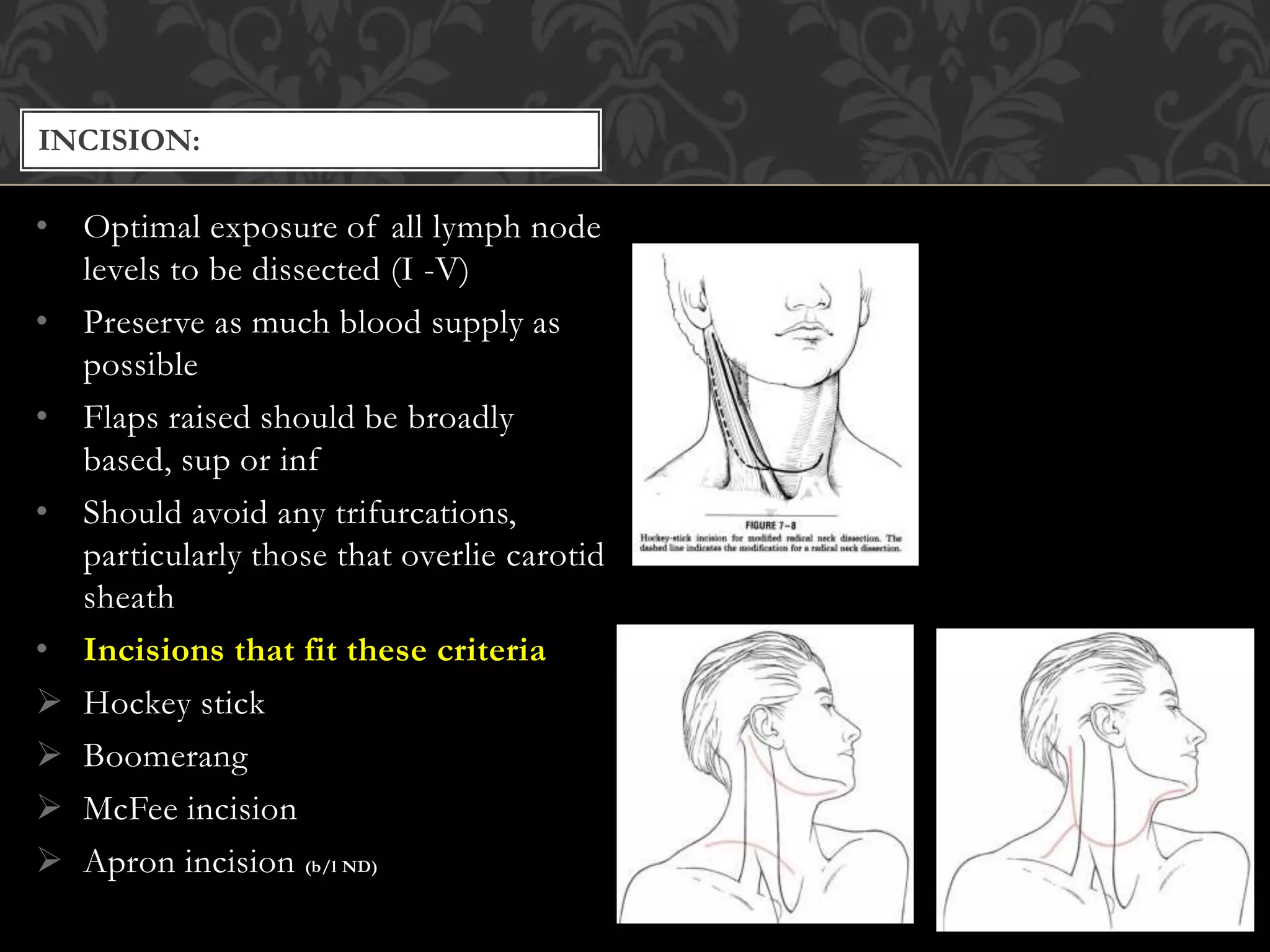
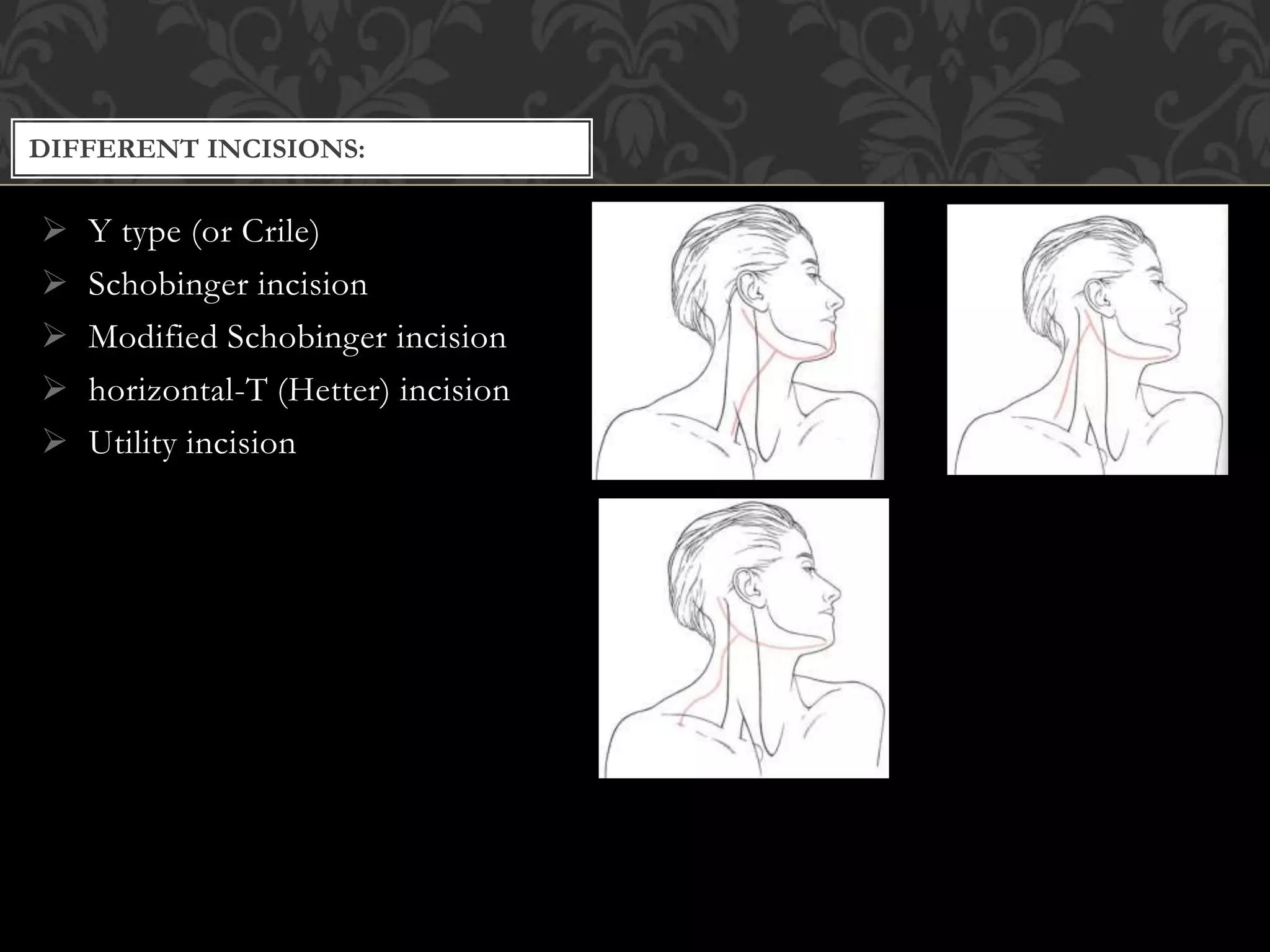
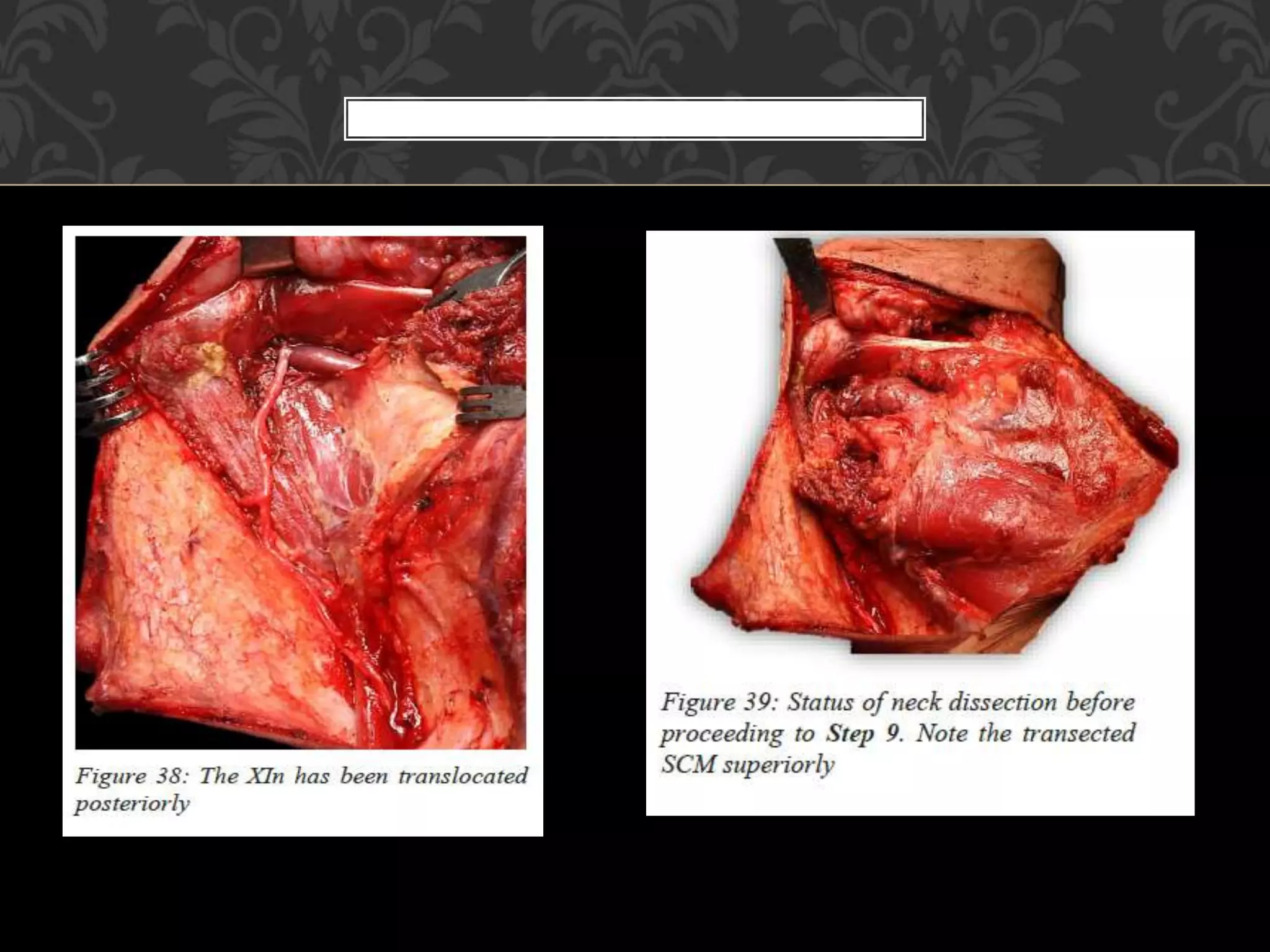
This document provides information about neck dissection procedures. It discusses the history and evolution of neck dissection, defines the different types of neck dissections including radical, modified radical and selective neck dissections, and describes the key steps in performing a modified radical neck dissection. Complications of neck dissection such as hemorrhage, wound infection, and carotid artery rupture are also summarized.