Embed presentation





















































































































































































































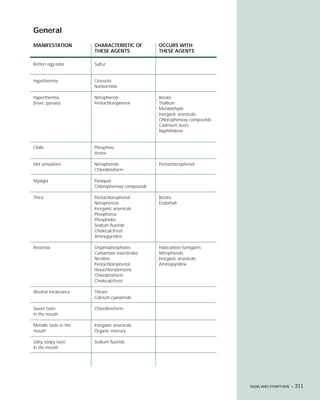
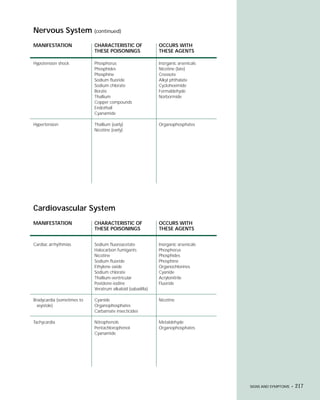
This document provides an introduction to the fifth edition of the manual "Recognition and Management of Pesticide Poisonings". The manual aims to provide health professionals with information on currently used pesticides and their health hazards, as well as recommendations for managing pesticide poisonings. Pesticide poisoning remains underdiagnosed, so the manual seeks to improve education of healthcare providers in this area. Key principles of pesticide poisoning management discussed include airway protection, gastric emptying procedures, use of activated charcoal and other decontamination methods, and hemodialysis or hemoperfusion for severe poisonings. Common pesticide exposures associated with poisonings are also summarized based on national surveillance data.