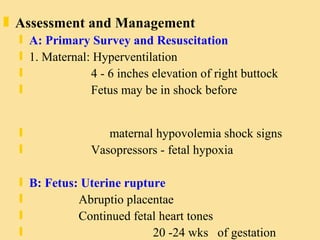
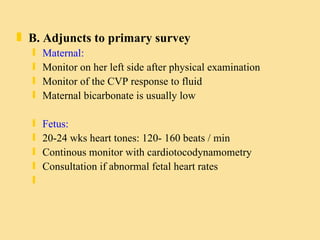
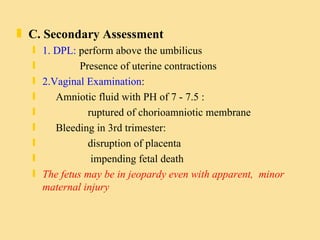
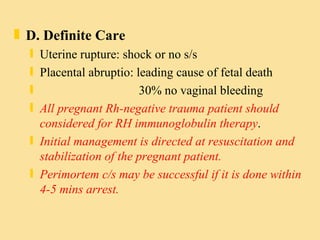
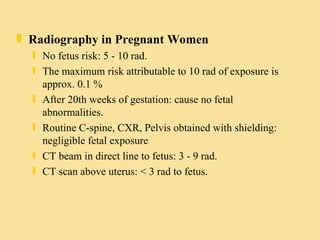
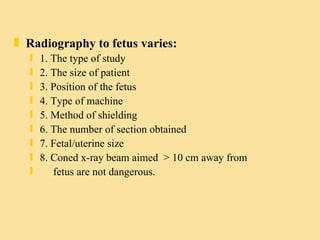
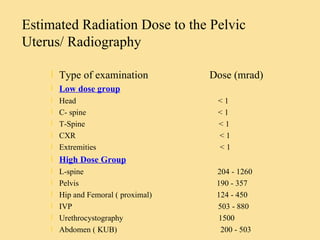
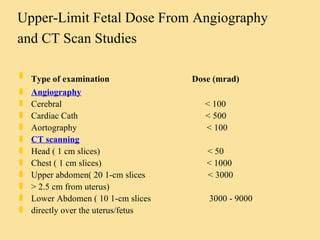
The document provides information on trauma in pregnant women, including anatomical and physiological changes during pregnancy, mechanisms of injury, assessment and management of trauma, and radiation exposure risks. It discusses increased blood volume and changes to respiratory and musculoskeletal systems during pregnancy. Primary survey focuses on stabilizing the mother while also monitoring the fetus. Secondary assessment includes pelvic exams and ultrasound. Definitive care depends on specific injuries like uterine rupture or placental abruption. Radiography risks to the fetus vary by gestational age, type of imaging, and shielding used.