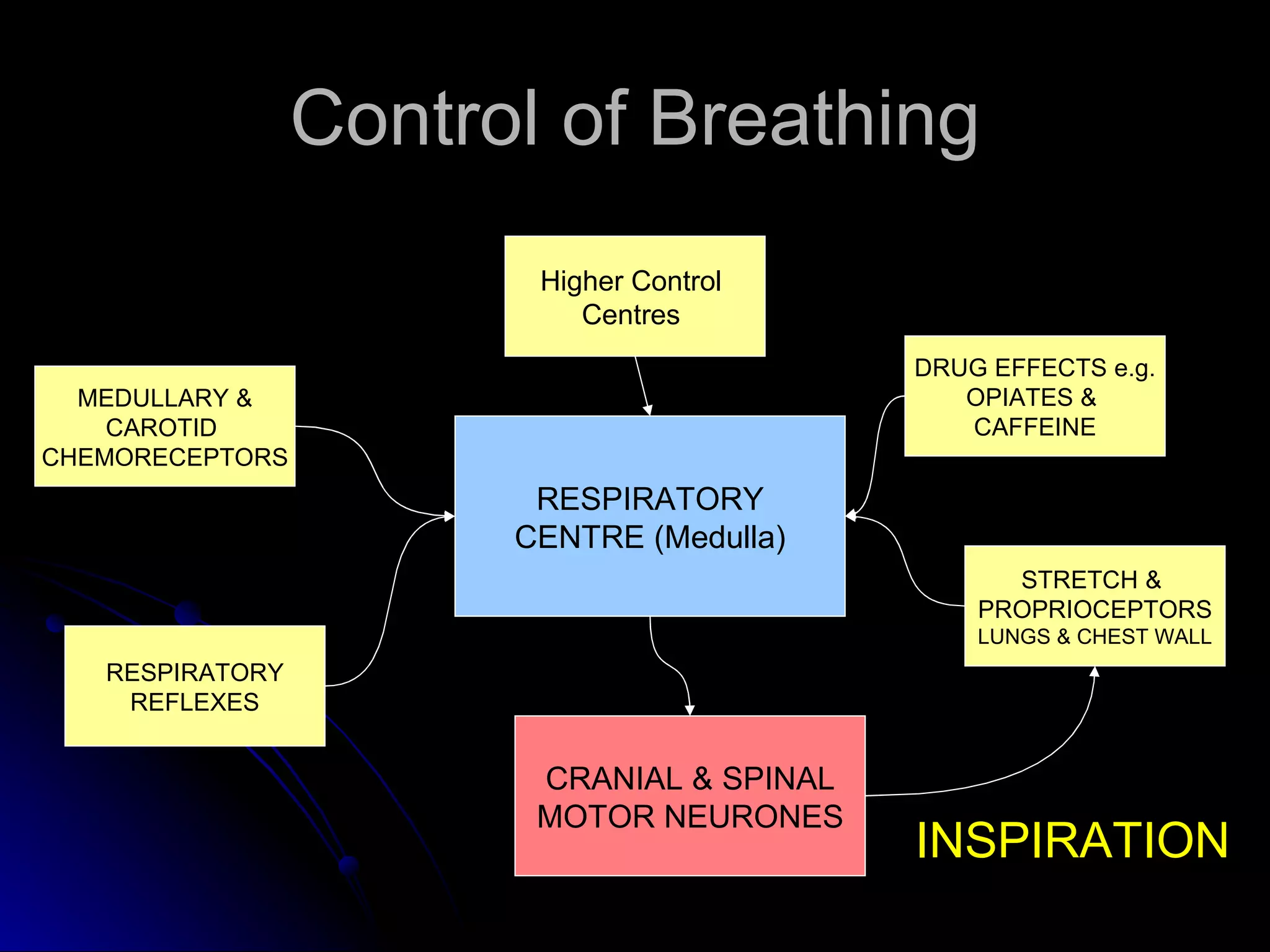
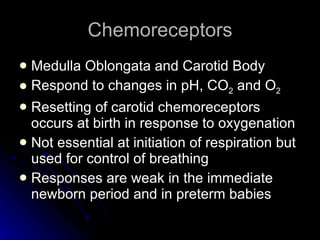
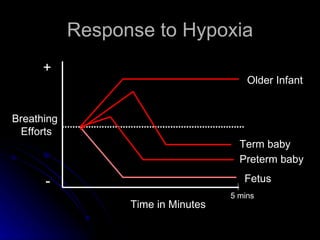
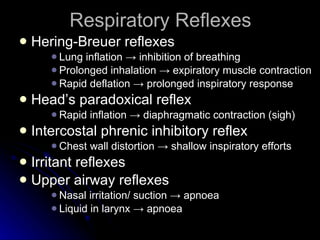
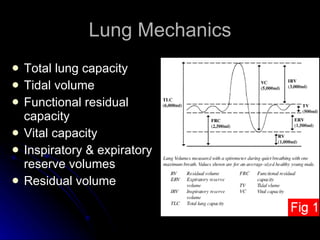
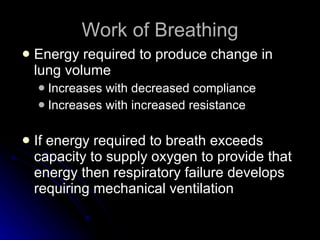
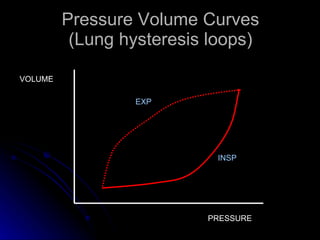
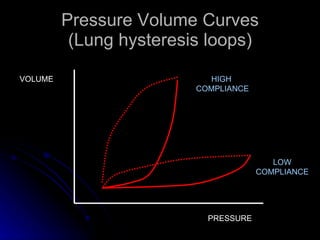
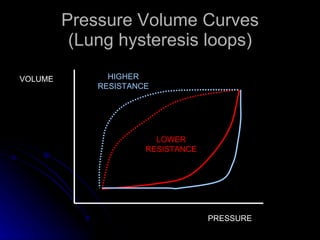
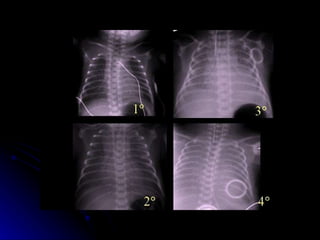
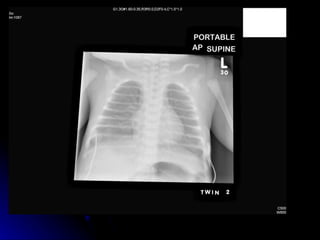
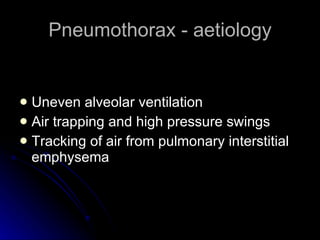
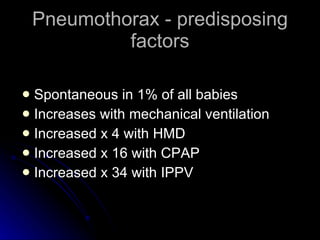
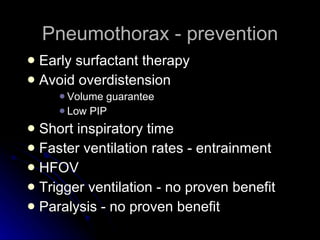
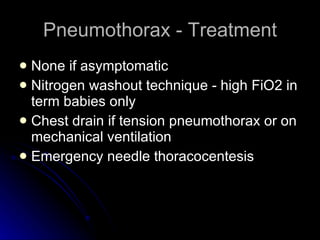
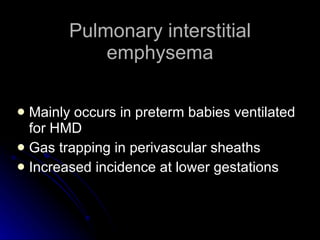
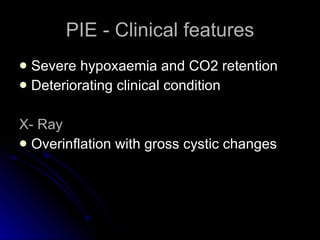
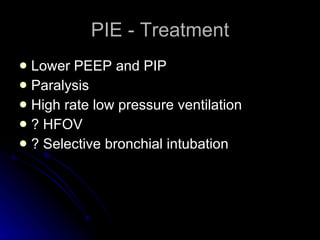
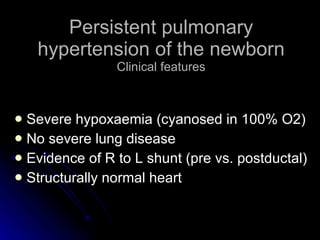
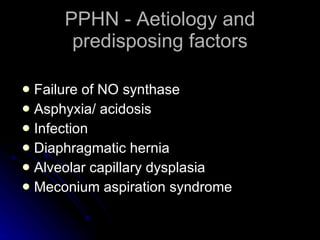
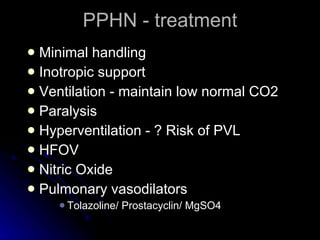
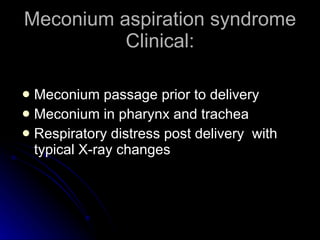
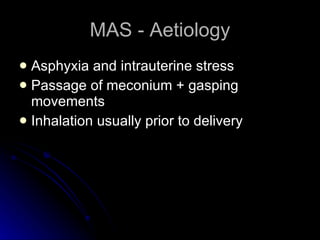
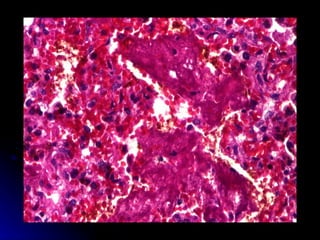
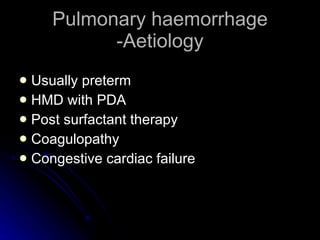
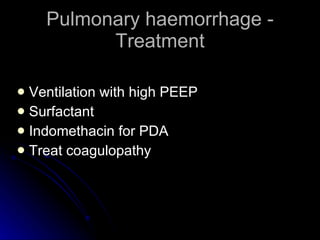
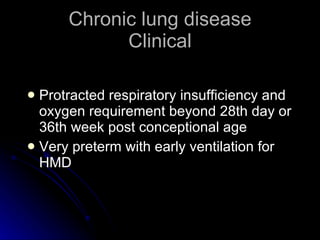
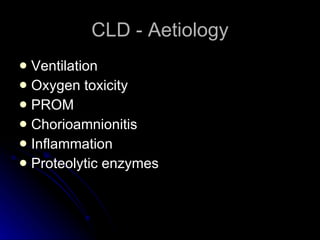
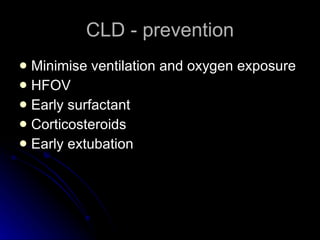
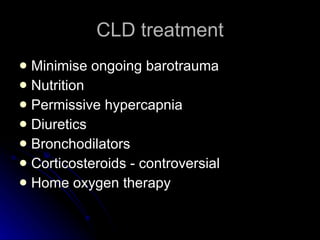
The document discusses control of breathing and neonatal respiratory diseases. It covers the respiratory center in the medulla, chemoreceptors, respiratory reflexes, lung mechanics, definitions of terms like tidal volume and compliance. It then summarizes several neonatal respiratory diseases like hyaline membrane disease, transient tachypnea of the newborn, pneumothorax, pulmonary interstitial emphysema, persistent pulmonary hypertension of the newborn, meconium aspiration syndrome, and chronic lung disease. For each disease it discusses clinical features, etiology, treatments and methods of prevention.