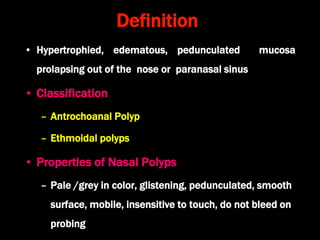
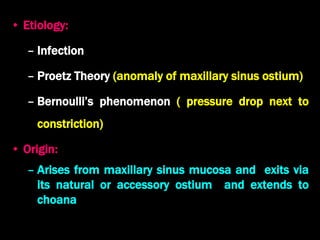
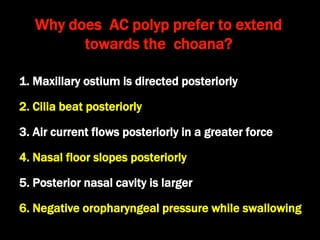
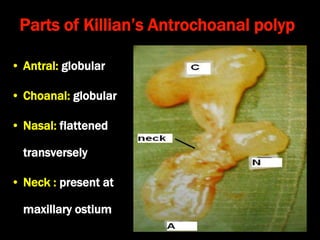
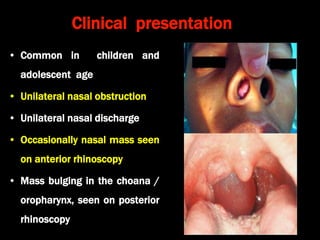
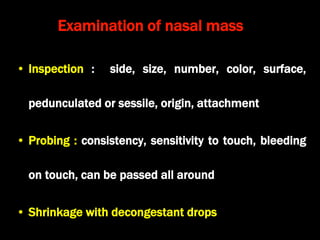
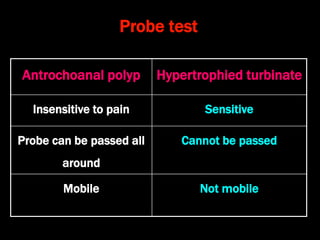
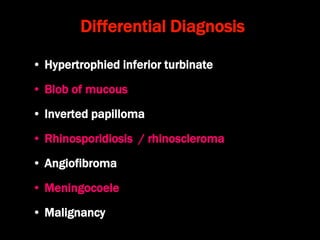
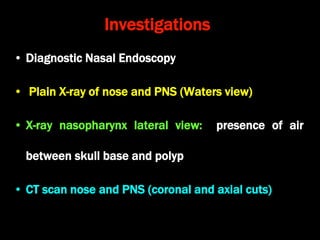
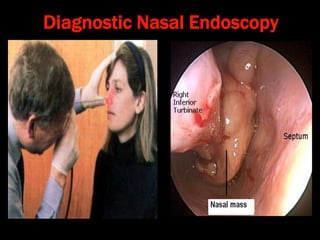
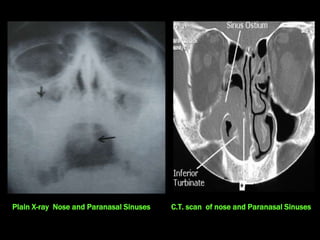
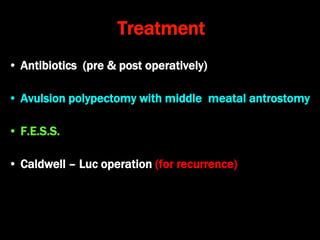
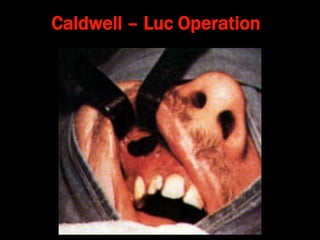
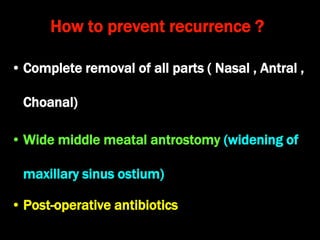
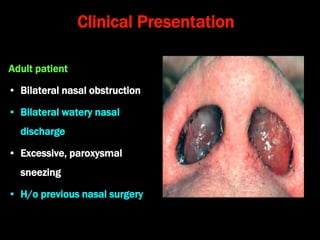
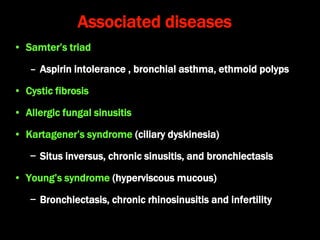
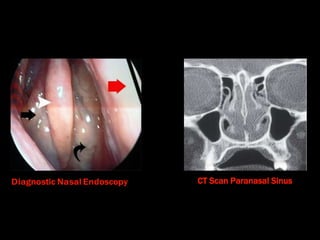
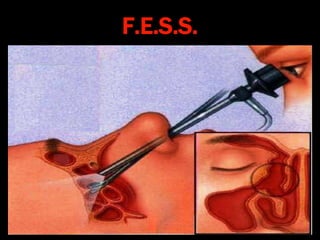
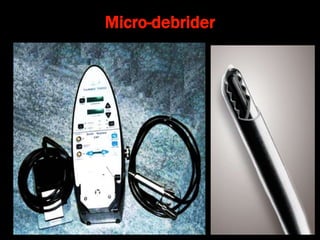
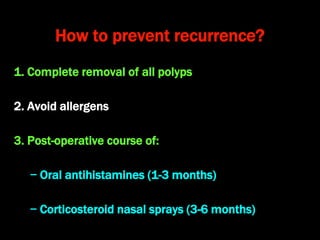
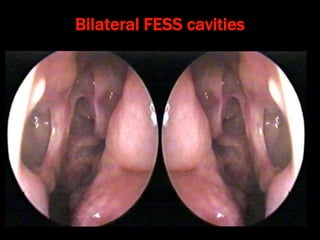
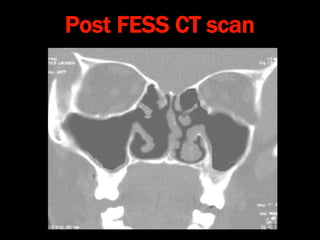
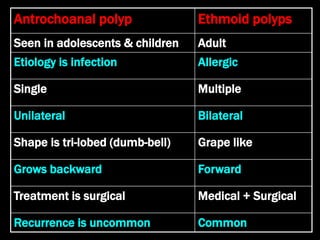
The document discusses nasal polyps, specifically antrochoanal and ethmoidal polyps, including their definitions, classifications, clinical presentations, and treatment options. It highlights the common symptoms in children and adults, the importance of diagnostic procedures like nasal endoscopy and CT scans, and various surgical and non-surgical treatments available. Preventive measures to reduce recurrence are also outlined, emphasizing complete removal and management of underlying conditions.