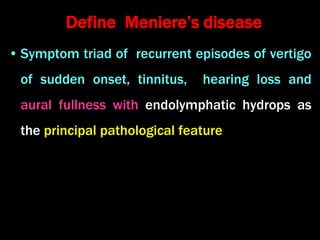
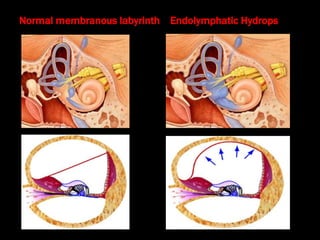
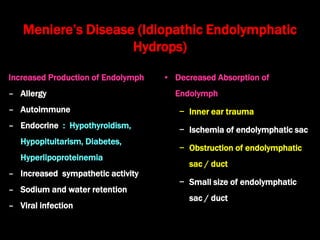
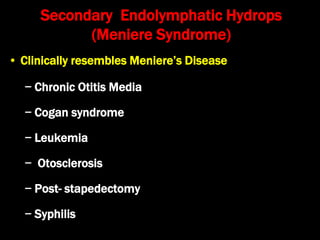
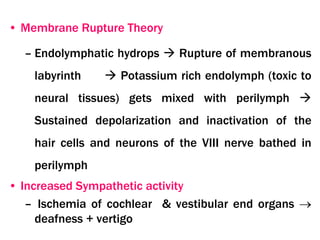
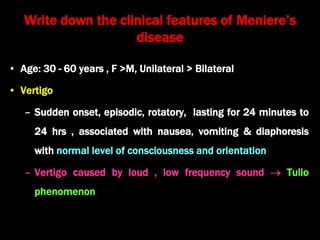
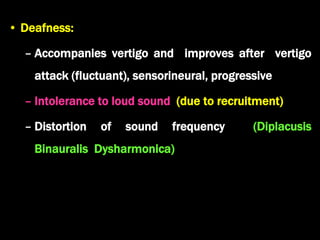
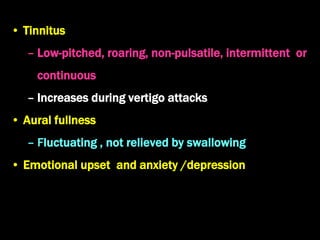
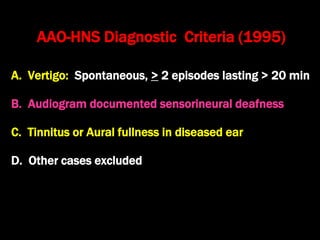
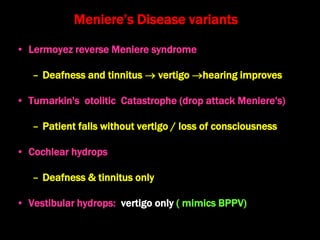
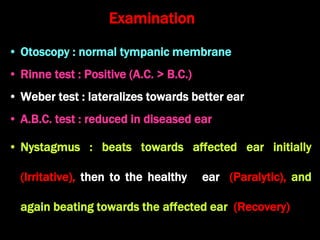
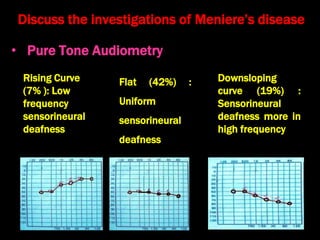
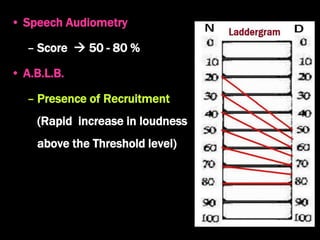
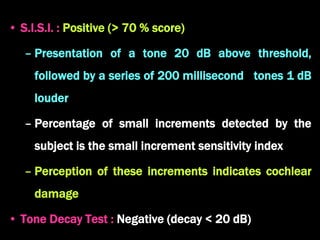
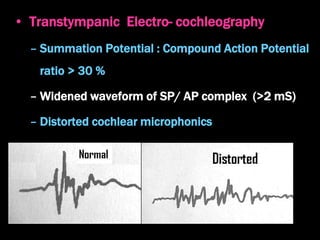
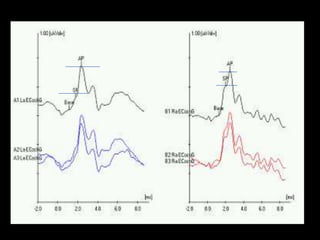
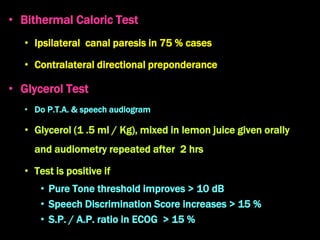
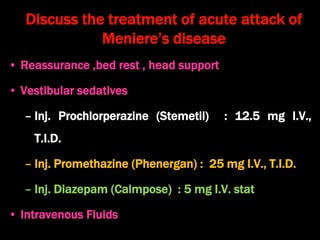
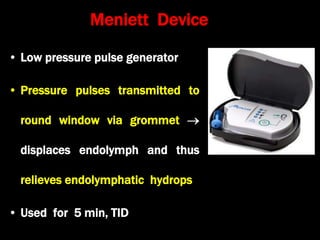
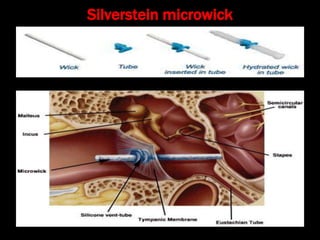
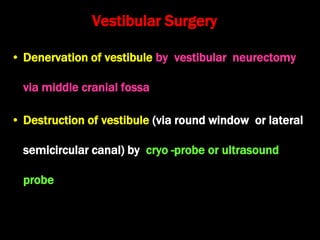
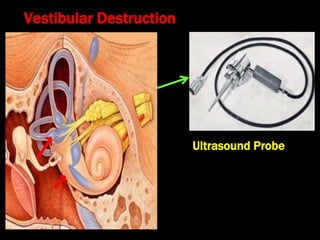
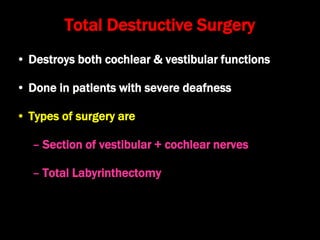
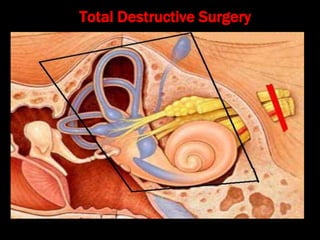
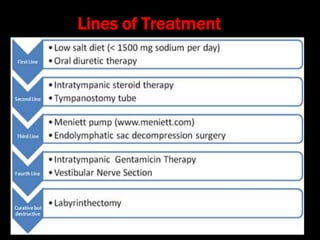
Meniere's disease is characterized by a triad of symptoms: recurrent vertigo, tinnitus, and hearing loss, linked to endolymphatic hydrops. It can arise from various etiological factors, including increased endolymph production and decreased absorption, leading to symptoms that fluctuate over time. Diagnosis relies on audiometric tests and clinical criteria, with treatment options ranging from dietary changes and medication to surgical interventions as necessary.