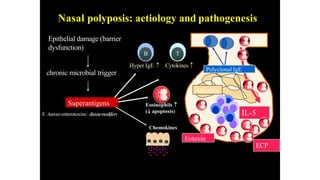
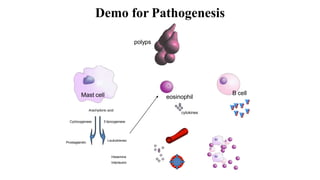
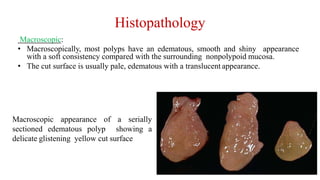
Nasal polyposis is a condition characterized by benign growths called polyps that develop in the nasal cavity and sinuses. The document discusses the epidemiology, etiology, pathogenesis, clinical presentation, diagnosis, and histopathology of nasal polyposis. Key points include:
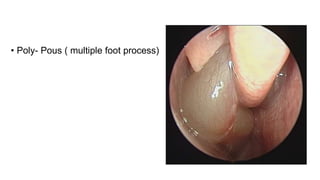
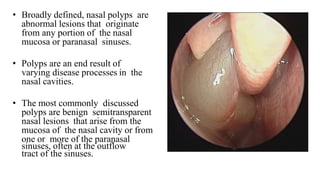
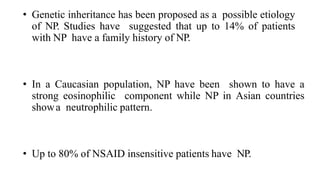
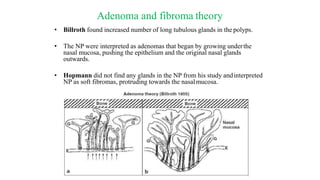
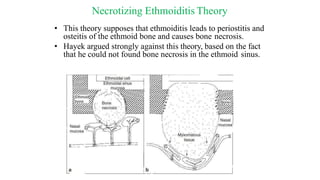
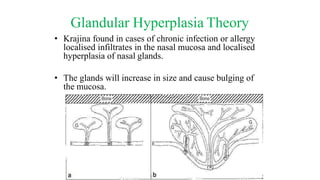
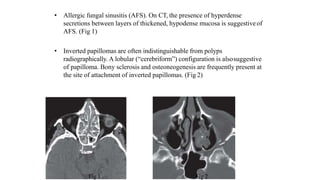
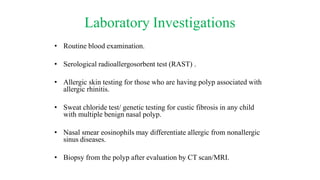
- Nasal polyps originate from the nasal mucosa and paranasal sinuses. Common causes include chronic sinus inflammation and allergy.
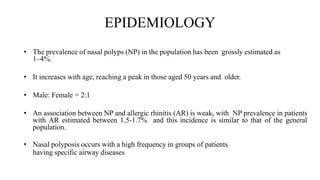
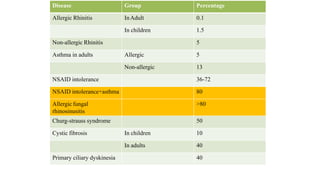
- Prevalence is 1-4% generally but higher in patients with asthma, cystic fibrosis, or aspirin sensitivity.
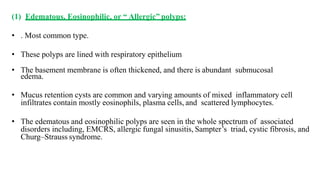
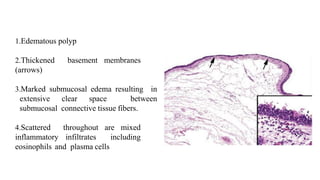
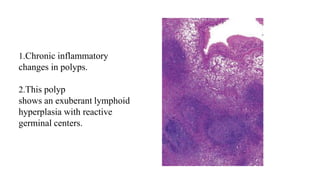
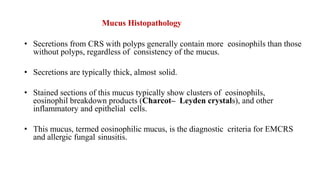
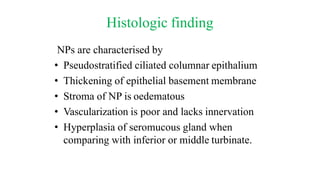
- Histopathology shows edematous polyps with eosinophils or chronic inflammatory polyps with fibrosis.
- Symptoms include nasal