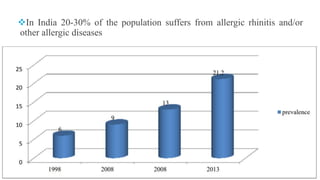
This document provides an overview of allergic rhinitis, including its definition, symptoms, epidemiology, etiology, pathophysiology, diagnosis, and treatment approaches. Some key points:
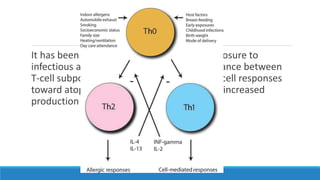
- Allergic rhinitis is an IgE-mediated inflammatory disease of the nose induced by exposure to allergens, characterized by symptoms like sneezing, nasal discharge, and congestion.
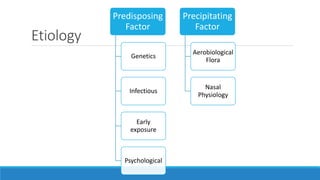
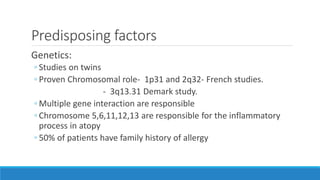
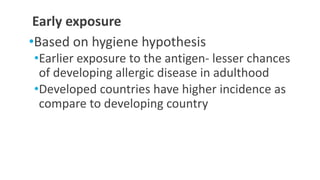
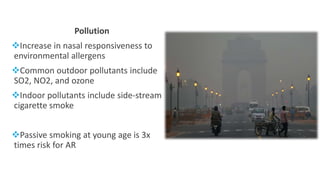
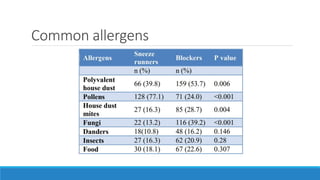
- Genetic and environmental factors like pollution, infections, and diet influence one's risk. Common allergens include dust mites, animal dander, and pollen.
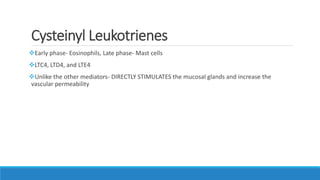
- Upon allergen exposure, IgE antibodies are produced, and subsequent exposures lead to degranulation of mast cells and basophils


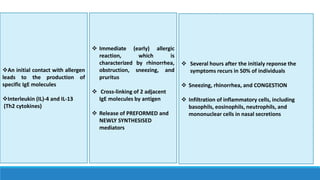
![Early response
Preformed Mediators
◦ Histamine
◦ Proteases [chymase and tryptase]
Newly synthesized
◦ Prostaglandins [PGDs]
◦ Cysteinyl leukotrienes[CysLTs]
◦ Platelet activating factor
◦ Bradykinin,
◦ Ils
◦ Tumor necrosis factor-α [TNF-α]
◦ Granulocyte- macrophage colony-stimulating factor)](https://image.slidesharecdn.com/allergicrhinitis-200413125400/85/Allergic-rhinitis-15-320.jpg)