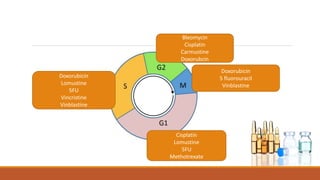
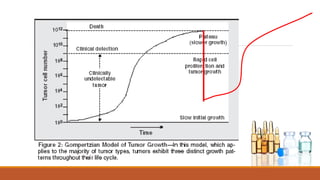
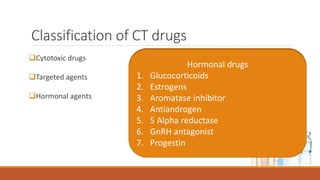
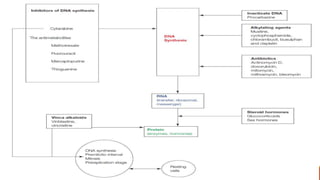
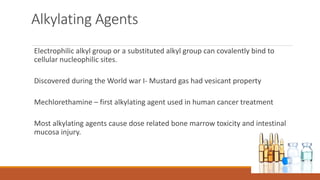
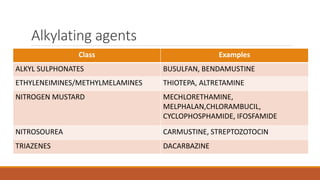
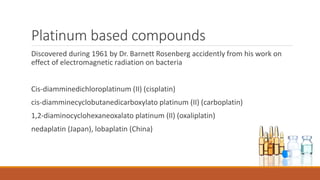
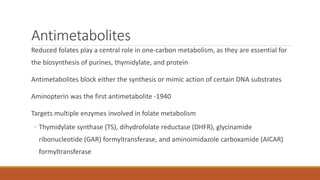
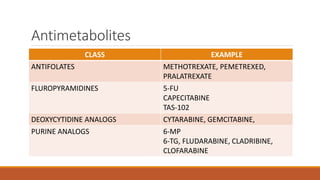
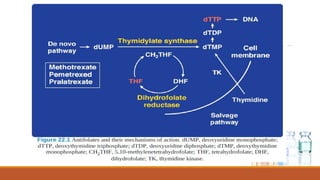
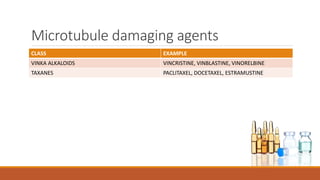
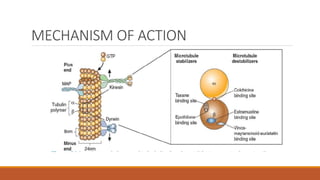
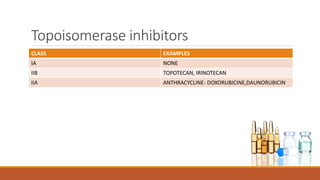
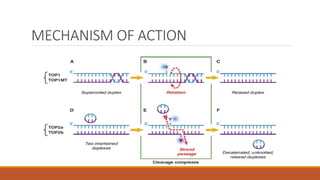
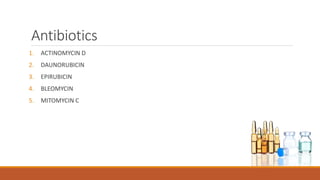
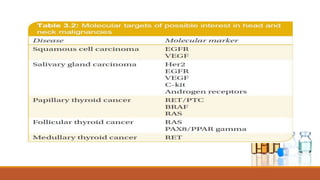
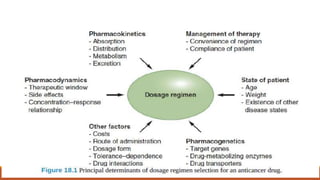
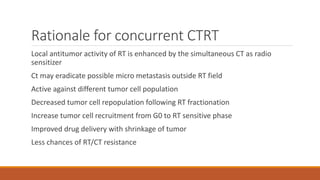
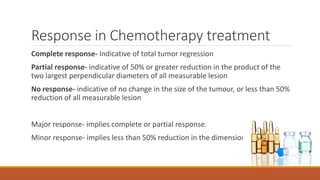
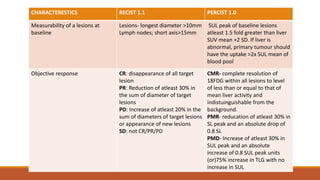
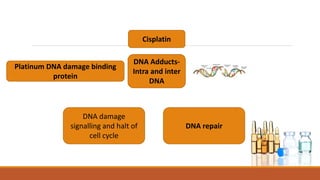
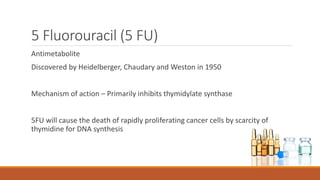
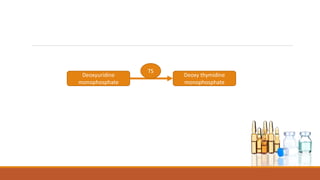
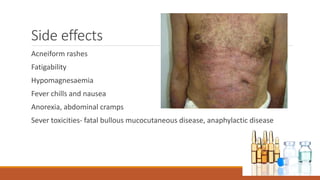
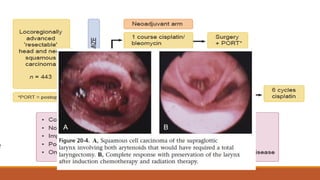
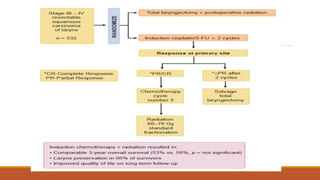
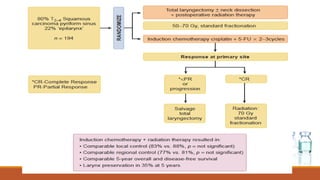
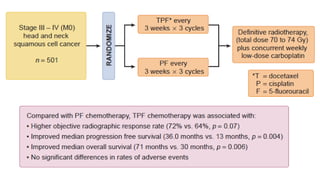
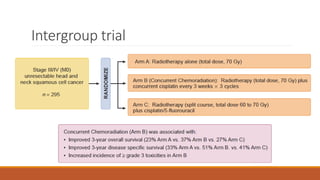
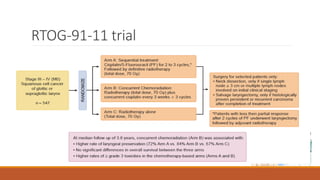
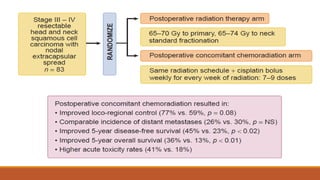
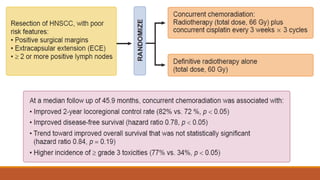
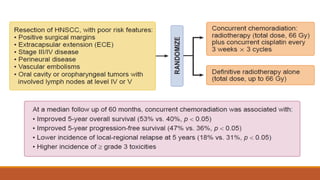
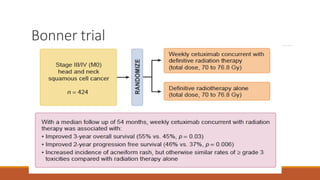
This document provides an overview of chemotherapy for head and neck cancer. It discusses the cell cycle effects of chemotherapy drugs and classifications including cytotoxic, targeted, and hormonal agents. Specific drugs are explained including mechanisms of action, indications, and side effects. The document also reviews landmark clinical trials establishing concurrent chemoradiotherapy as the standard of care for locally advanced head and neck cancer. Targeted agents like cetuximab are now being used for recurrent/metastatic disease.