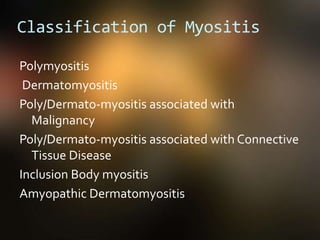
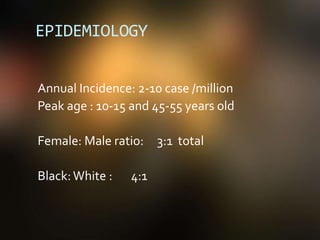
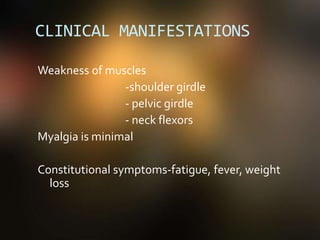
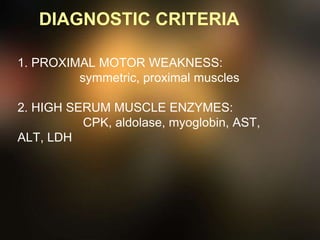
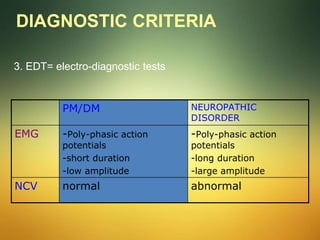
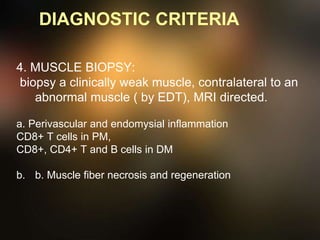
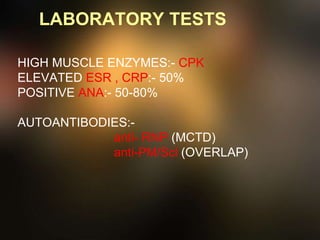
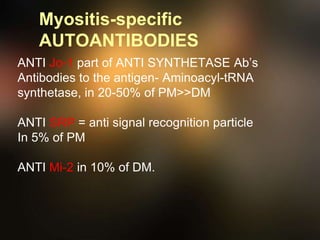
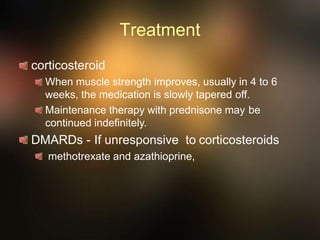
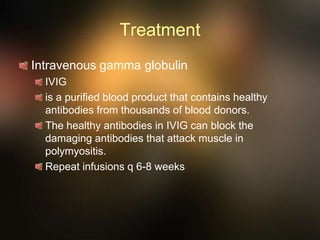
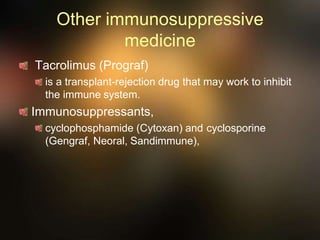
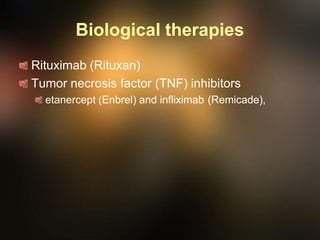
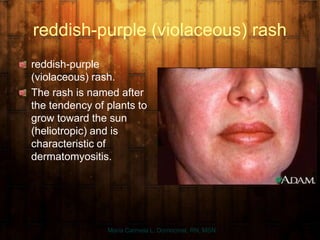
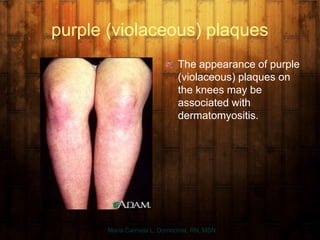
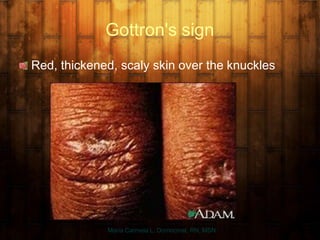
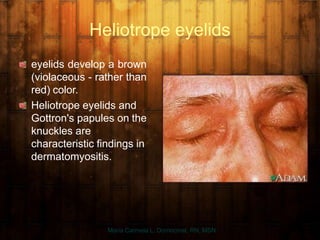
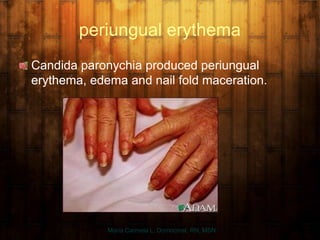
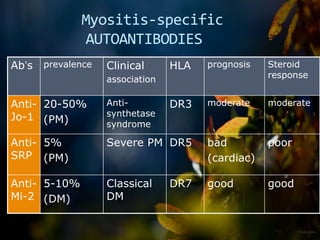
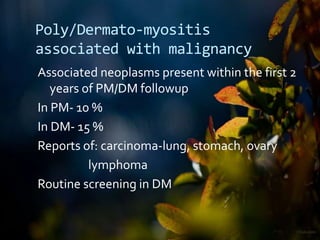
Myositis is defined as a slowly progressive inflammatory muscle disease characterized by symmetrical weakness, primarily affecting proximal limb and trunk muscles. Polymyositis and dermatomyositis are key classifications, each with specific symptoms, associated conditions, and diagnostic criteria, including muscle weakness, inflammatory markers, and muscle biopsy results. Treatment often involves corticosteroids, immunosuppressive agents, and management of associated complications, with varying prognoses depending on the form and associated conditions.