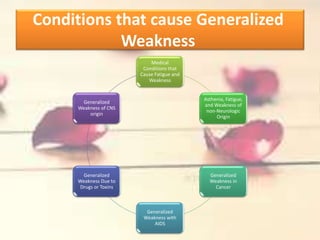
The document discusses various medical conditions that can cause generalized weakness, including:
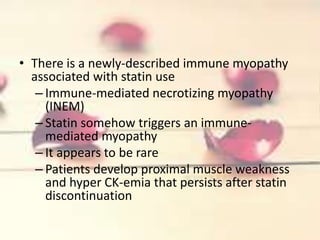
1) Psychiatric illnesses like depression which can cause perceived weakness; cardiovascular, hematologic, renal, pulmonary, and endocrine conditions; and medications like steroids, alcohol, statins, and colchicine.
2) Inflammatory myopathies like polymyositis, dermatomyositis, and inclusion body myositis are also covered - they differ in presentation, associated features, prognosis and response to treatment.
3) Evaluation for an unknown cause of weakness includes blood tests to check for conditions like anemia and thyroid/kidney problems.