Embed presentation
Downloaded 184 times
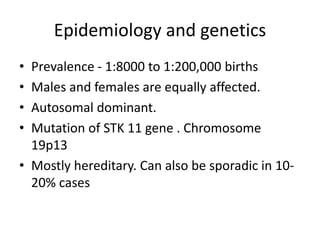
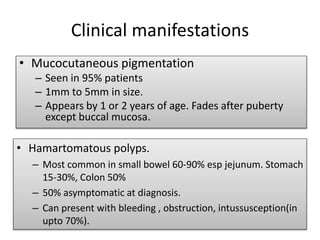
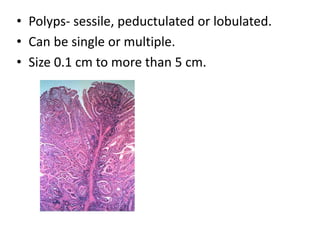
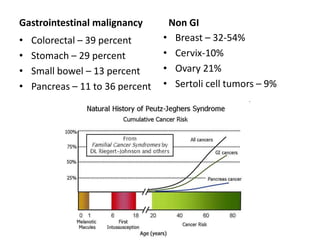
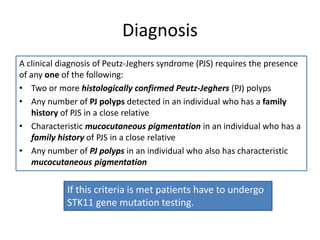
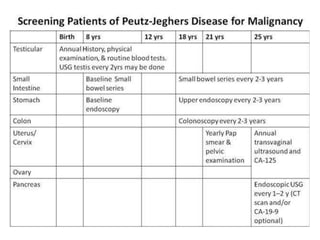

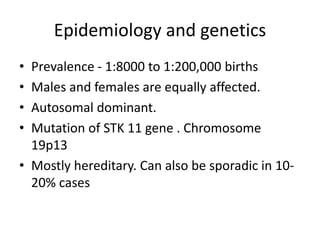
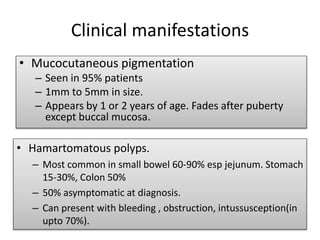
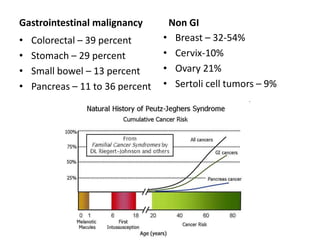
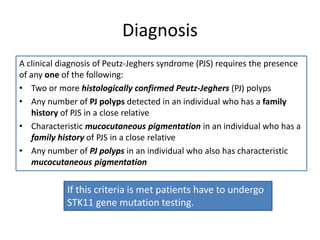
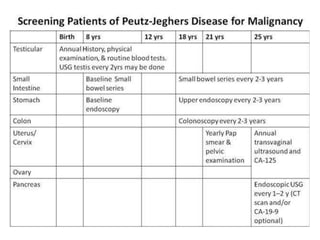
Peutz-Jeghers syndrome is a rare, autosomal dominant genetic disorder characterized by hamartomatous polyps in the gastrointestinal tract and pigmented lesions on the skin. It is caused by a mutation in the STK11 gene. People with PJS are at increased risk of cancers of the gastrointestinal tract as well as other organs. Management involves endoscopic screening and removal of polyps to prevent cancer complications.