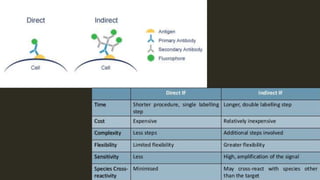
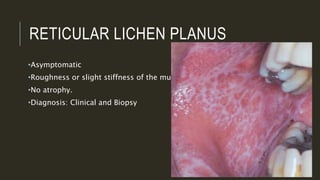
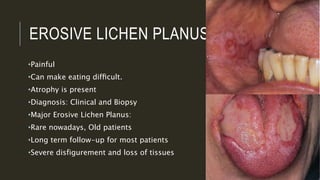
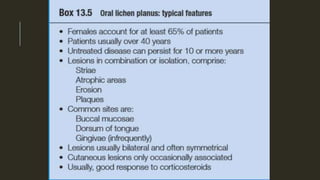
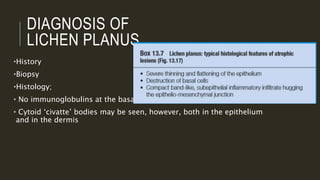
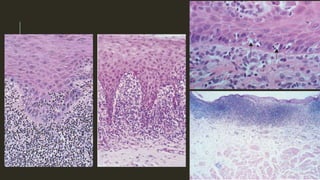
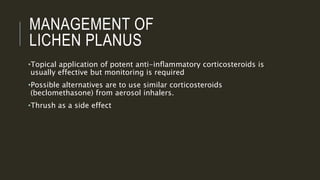
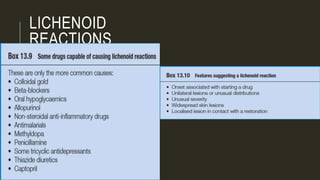
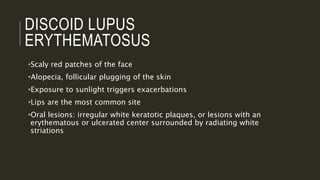
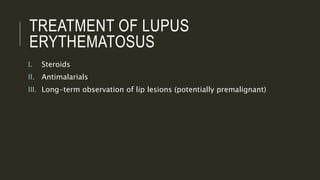
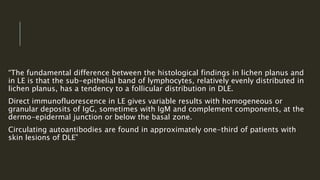
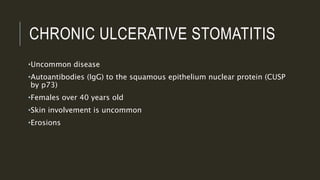
This document outlines several mucocutaneous diseases that can present in the oral cavity, including lichen planus, lupus erythematosus, chronic ulcerative stomatitis, and pemphigus vulgaris. It discusses the differences between oral and skin lesions, diagnostic tests like immunofluorescence, and the clinical features and management of these conditions. Key histological findings that can help differentiate lichen planus from lupus erythematosus are mentioned.