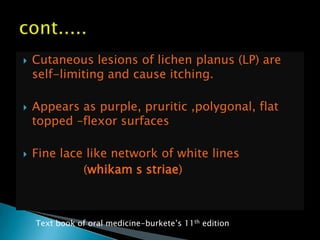
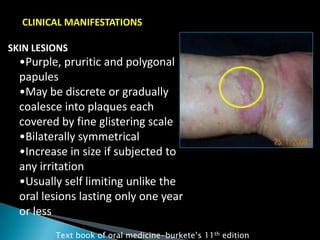
- Lichen planus is a chronic inflammatory disease that affects the skin, hair, nails and mucous membranes. It is characterized by pruritic papules and plaques with fine white lines or lacelike patterns.
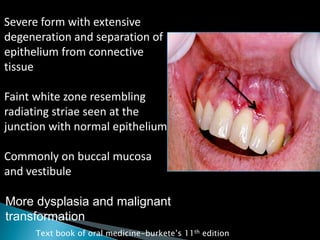
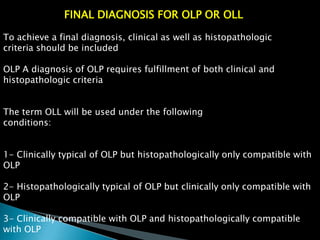
- Oral lichen planus (OLP) is a common form that affects the oral mucosa. It can present as reticular, papular, plaque-like, atrophic or erosive lesions, most often involving the buccal mucosa.
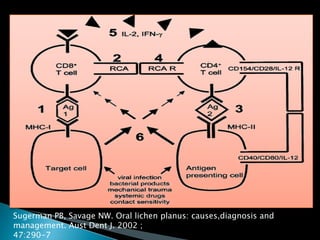
- Histopathology reveals hyperkeratosis, acanthosis, saw-toothed rete pegs, liquefaction degeneration of the basal layer and a band-like lymphocytic infiltrate in the superficial lam