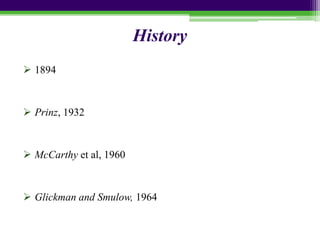
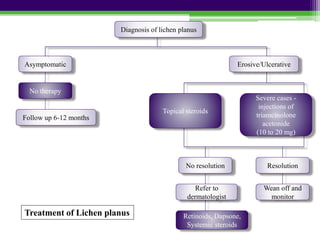
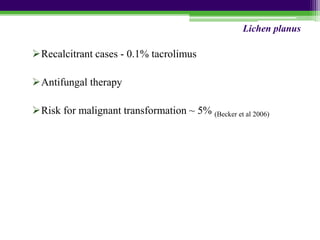
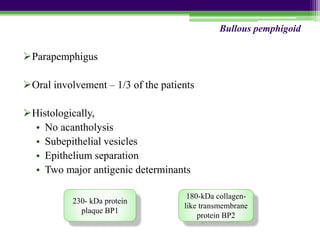
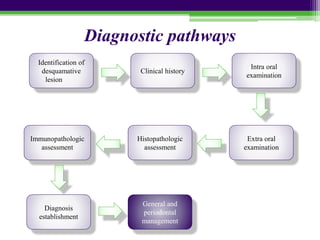
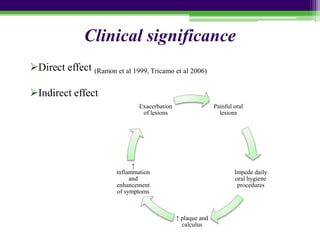
This document provides an overview of desquamative gingivitis, a group of immune-mediated disorders that cause inflammation and sloughing of the gingival epithelium. It discusses the classification, associated disorders like lichen planus and pemphigoid, clinical presentation, histopathology, diagnosis and treatment. Desquamative gingivitis can be caused by conditions like mucous membrane pemphigoid, lichen planus, and pemphigus vulgaris. It is characterized by red, swollen gingiva with areas of denudation and vesicles. Diagnosis involves clinical evaluation, histopathology, and immunopathology testing. Management depends on the underlying disorder but may include top