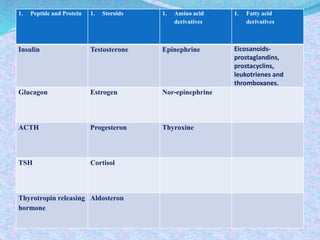
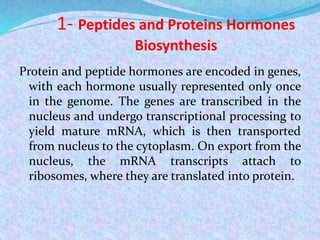
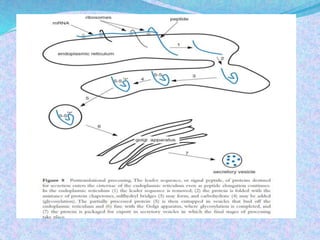
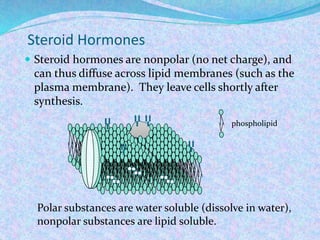
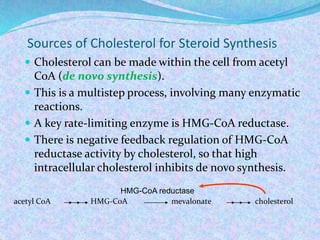
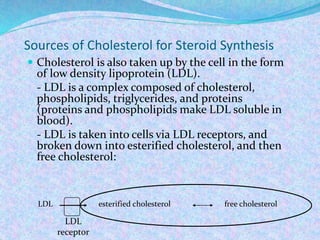
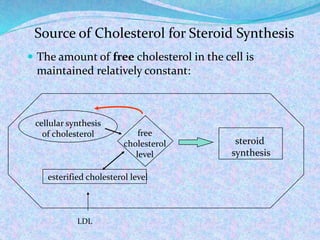
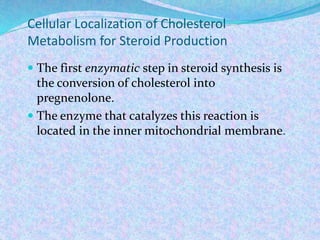
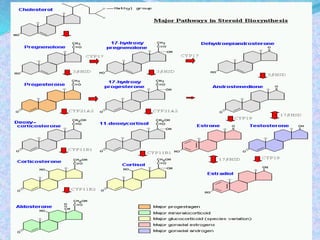
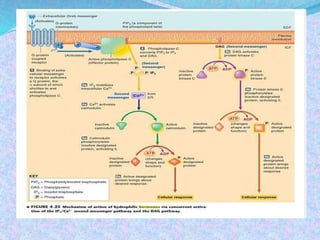
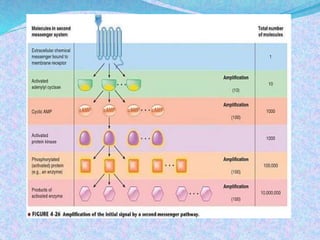
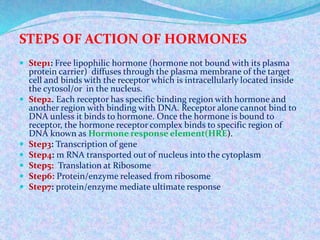
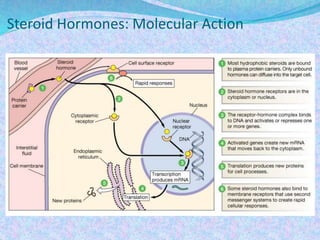
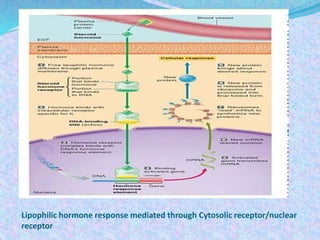
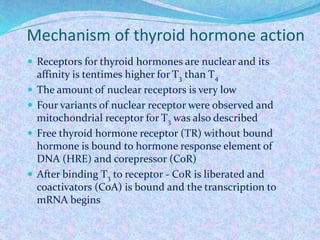
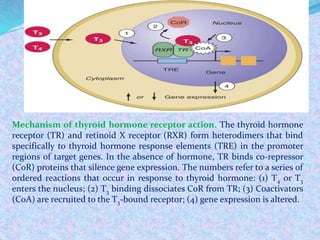
This document summarizes the biosynthesis of the main categories of hormones: peptides and proteins, steroids, amino acid derivatives, and fatty acid derivatives. It discusses the processes of gene transcription and translation that produce peptide hormones. It explains how steroid hormones are derived from cholesterol in the mitochondria, and their lipid solubility allows diffusion into target cells. Amino acid derivatives include thyroid hormones and catecholamines from tyrosine. Fatty acid derivatives include eicosanoids like prostaglandins. The document also summarizes the mechanisms of action for hydrophilic and lipophilic hormones, including cell surface receptors and nuclear receptors, and signal transduction pathways.