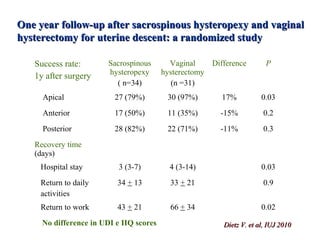
This document discusses several studies comparing prolapse repair surgery with and without hysterectomy. It notes that while hysterectomy is commonly performed during prolapse surgery, there is no evidence it improves repair durability. Studies found higher morbidity and new urinary, bowel, and sexual dysfunction with hysterectomy. For apical prolapse, sacrospinous hysteropexy and Manchester repair had fewer recurrences than vaginal hysterectomy. Uterine preservation was associated with shorter recovery time. Other topics discussed include rates of endometrial pathology found during hysterectomy, effects of hysterectomy on urinary incontinence and sexual function, and reasons for considering uterine preservation.