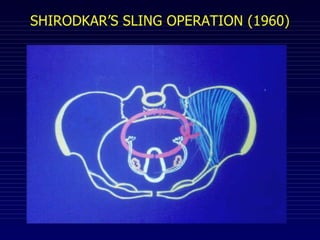
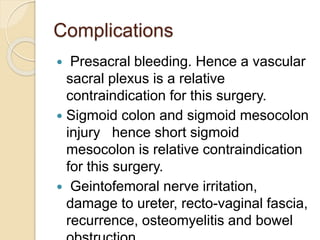
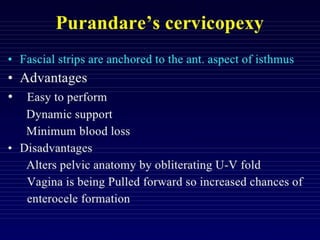
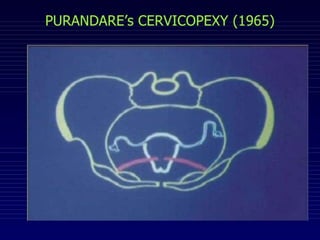
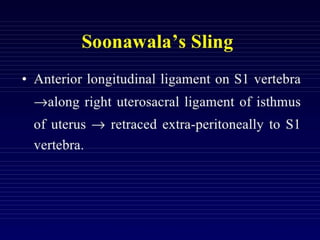
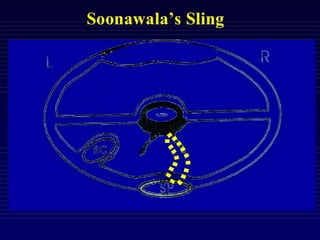
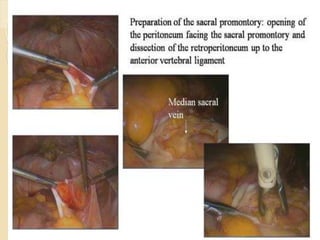
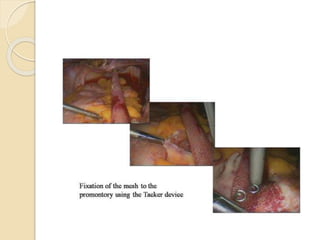
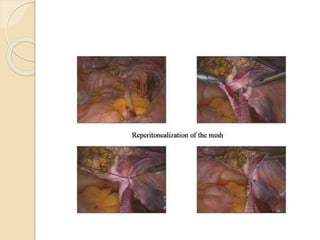
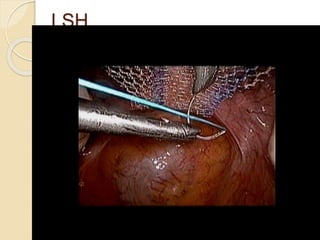
The document discusses various uterus sparing techniques for prolapse surgery in young women who desire to preserve fertility and menstrual function. It describes Shirodkar's sling operation, which has been shown to have high rates of normal vaginal delivery and low recurrence rates of prolapse. Laparoscopic sacrohysteropexy is indicated for young women with prolapse as it has better efficacy than vaginal sacrospinous fixation and results in fewer mesh complications compared to sacral colpopexy with hysterectomy. While sacral colpopexy has high success rates, it also carries risks of serious mesh-related complications requiring reoperation years later.