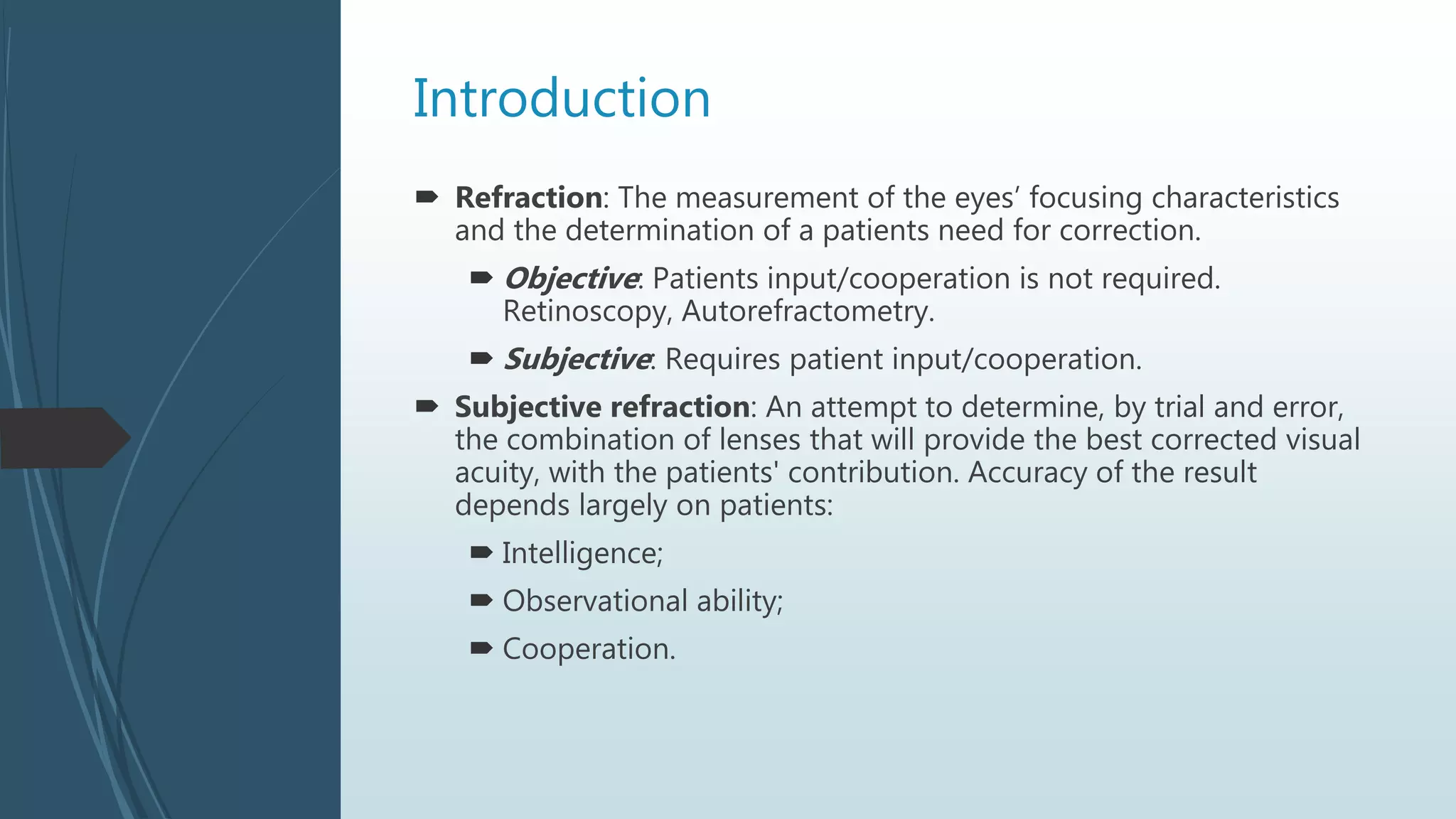
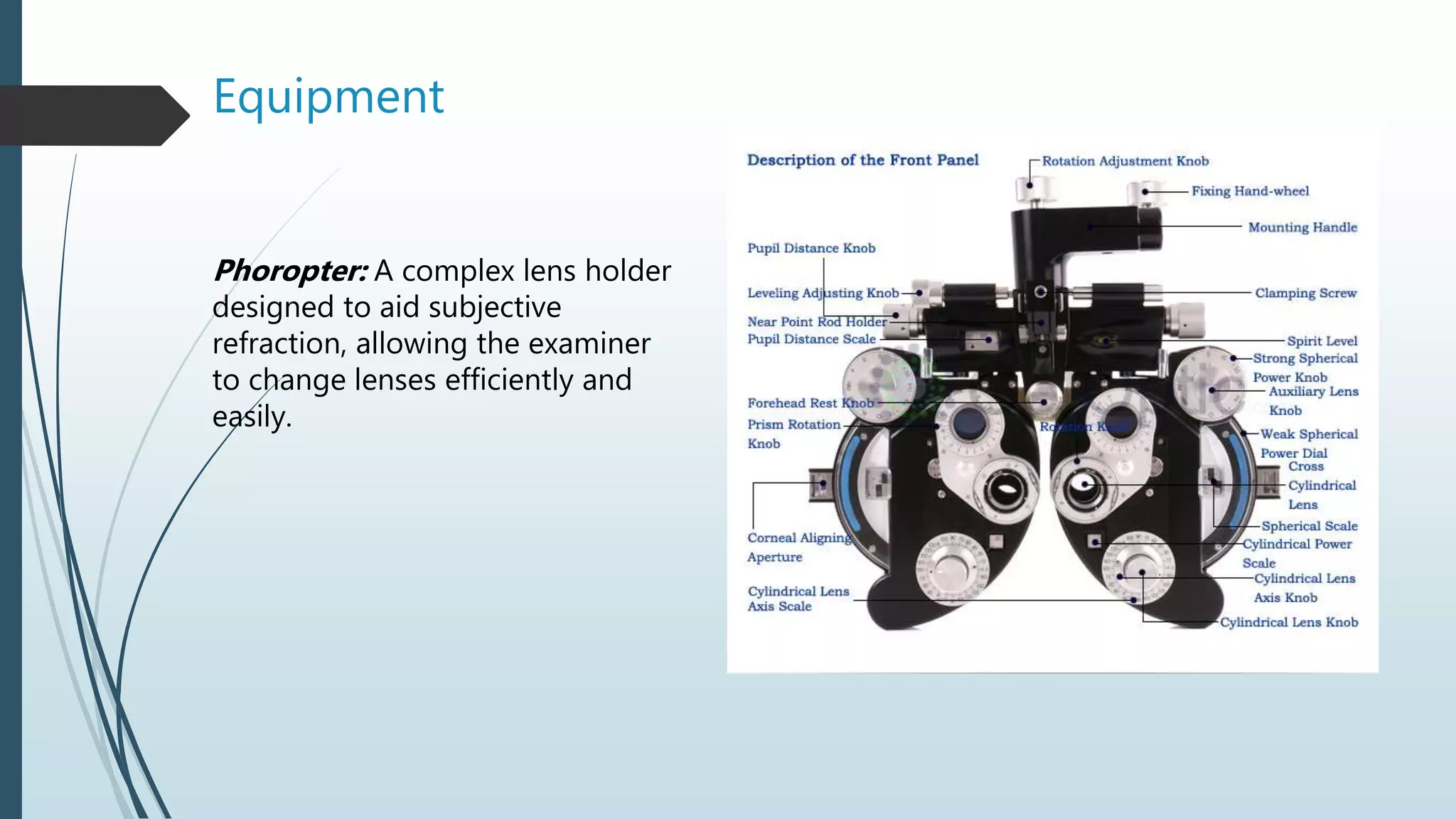
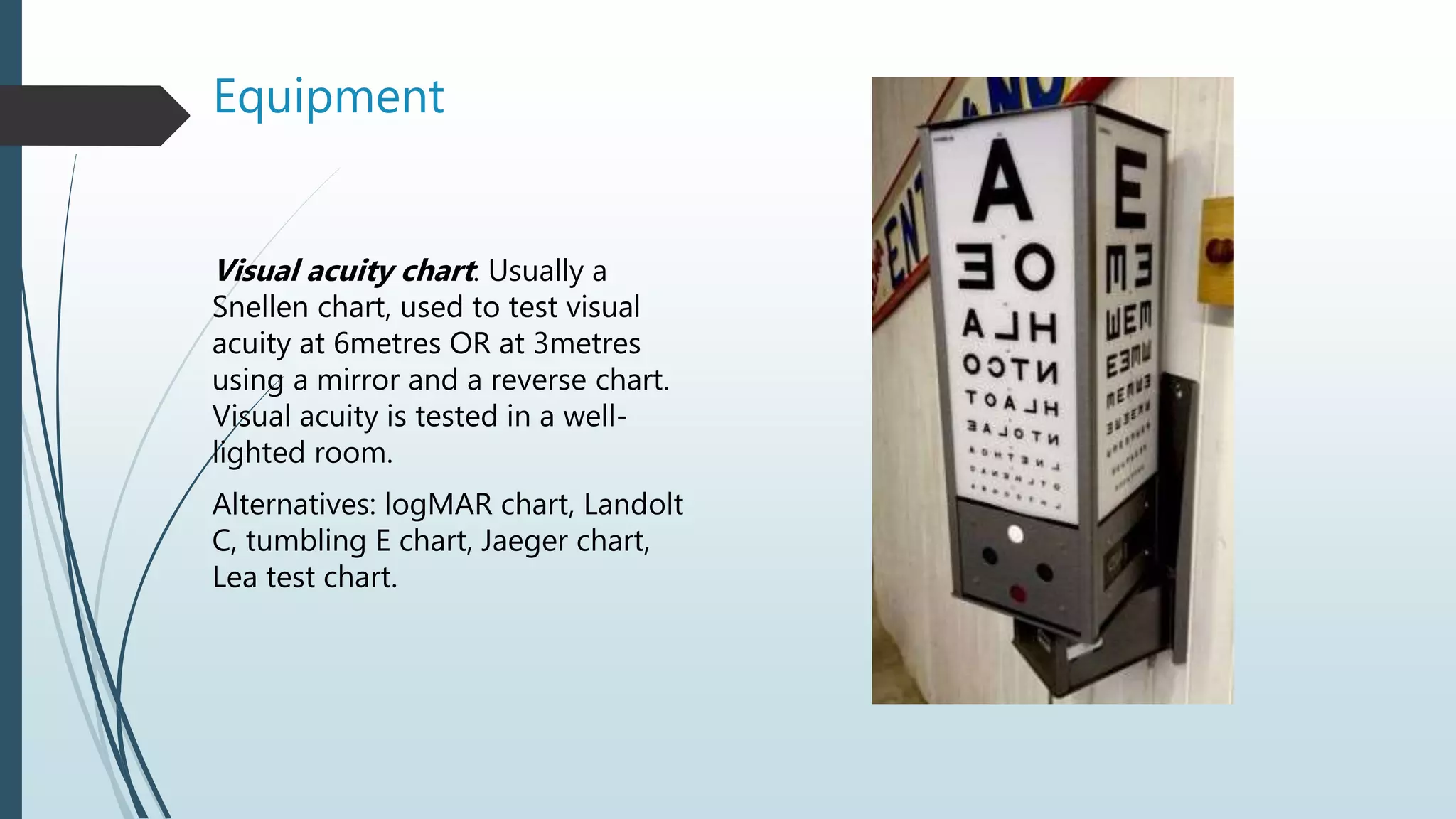
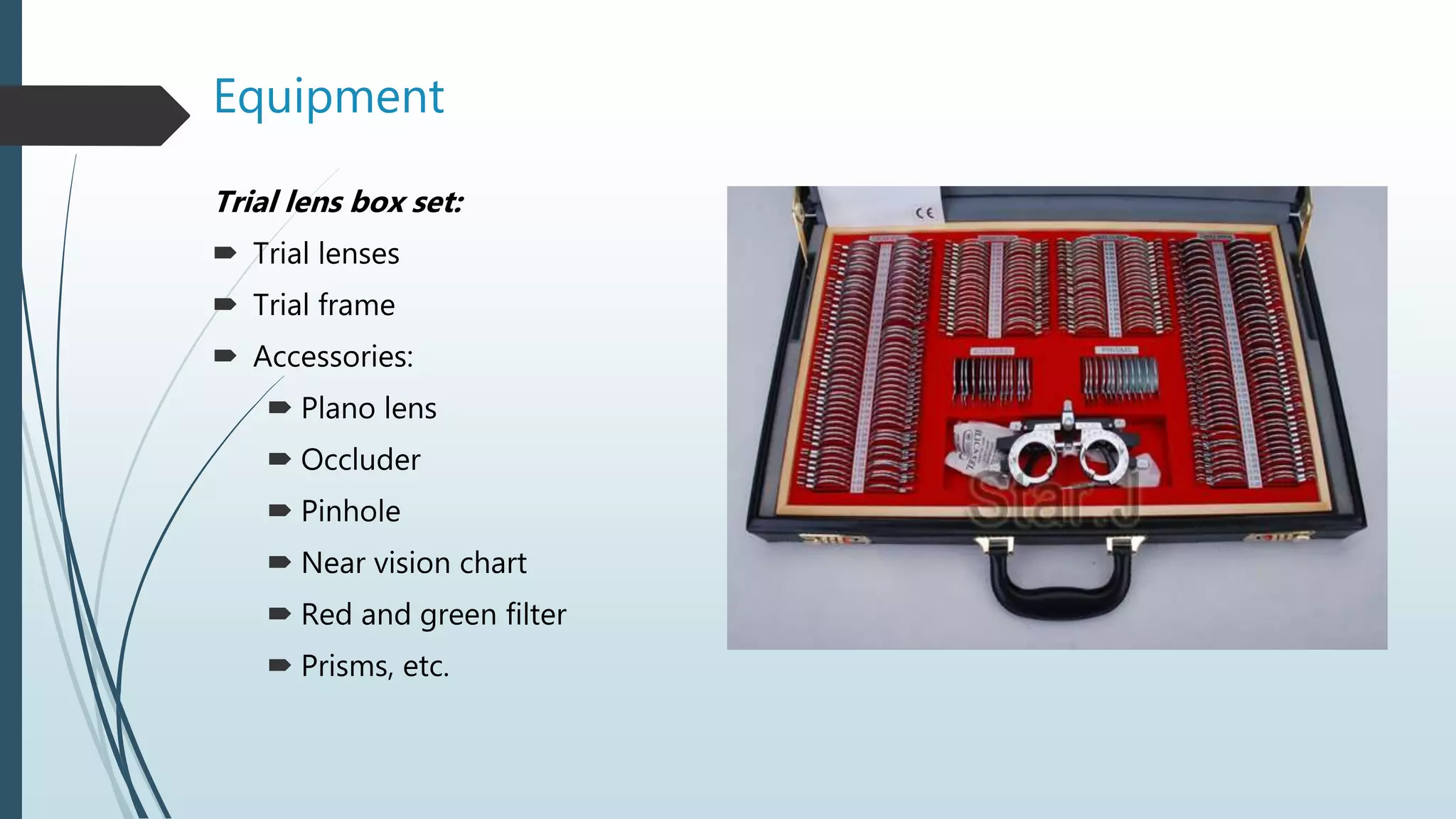
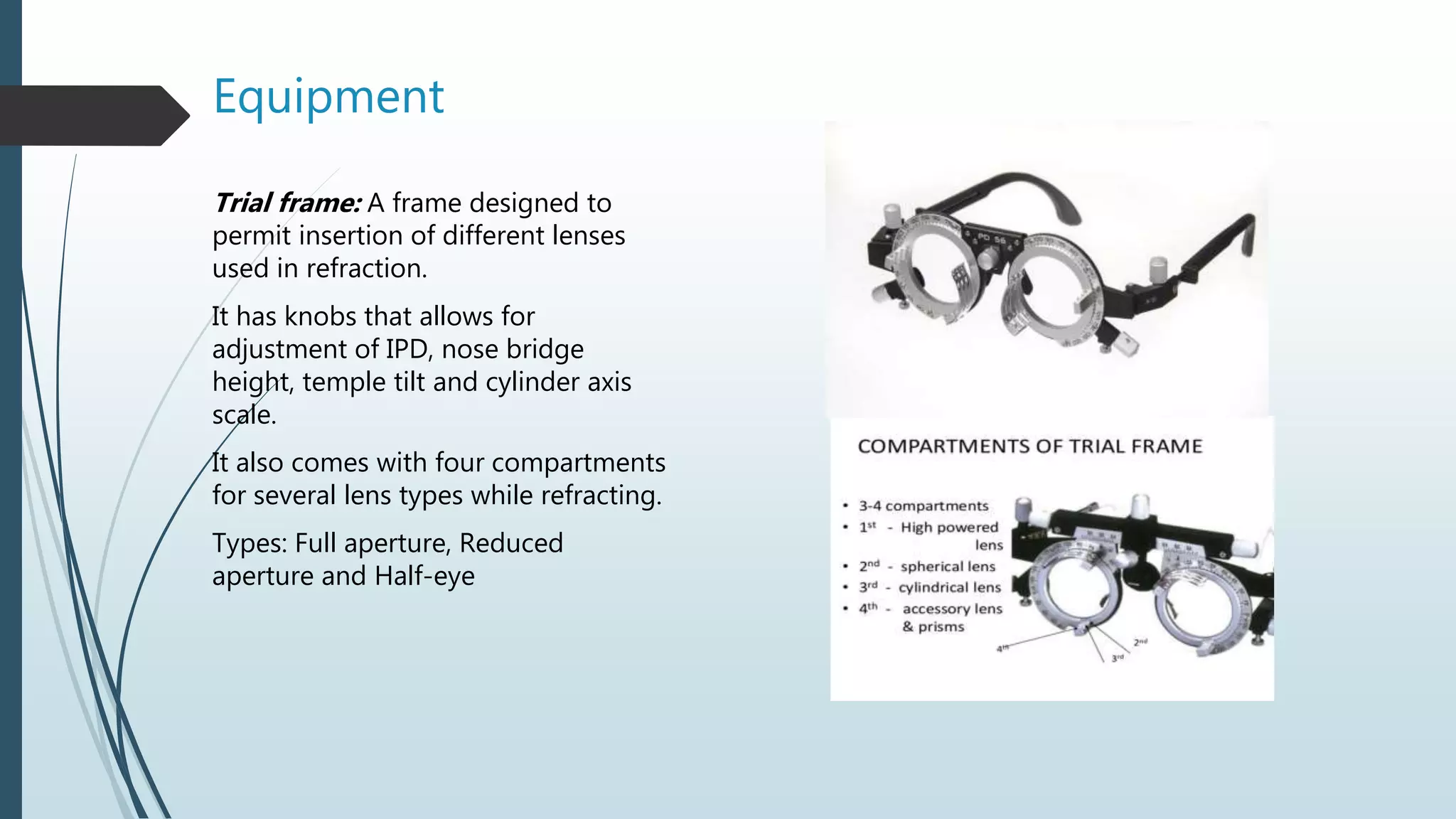
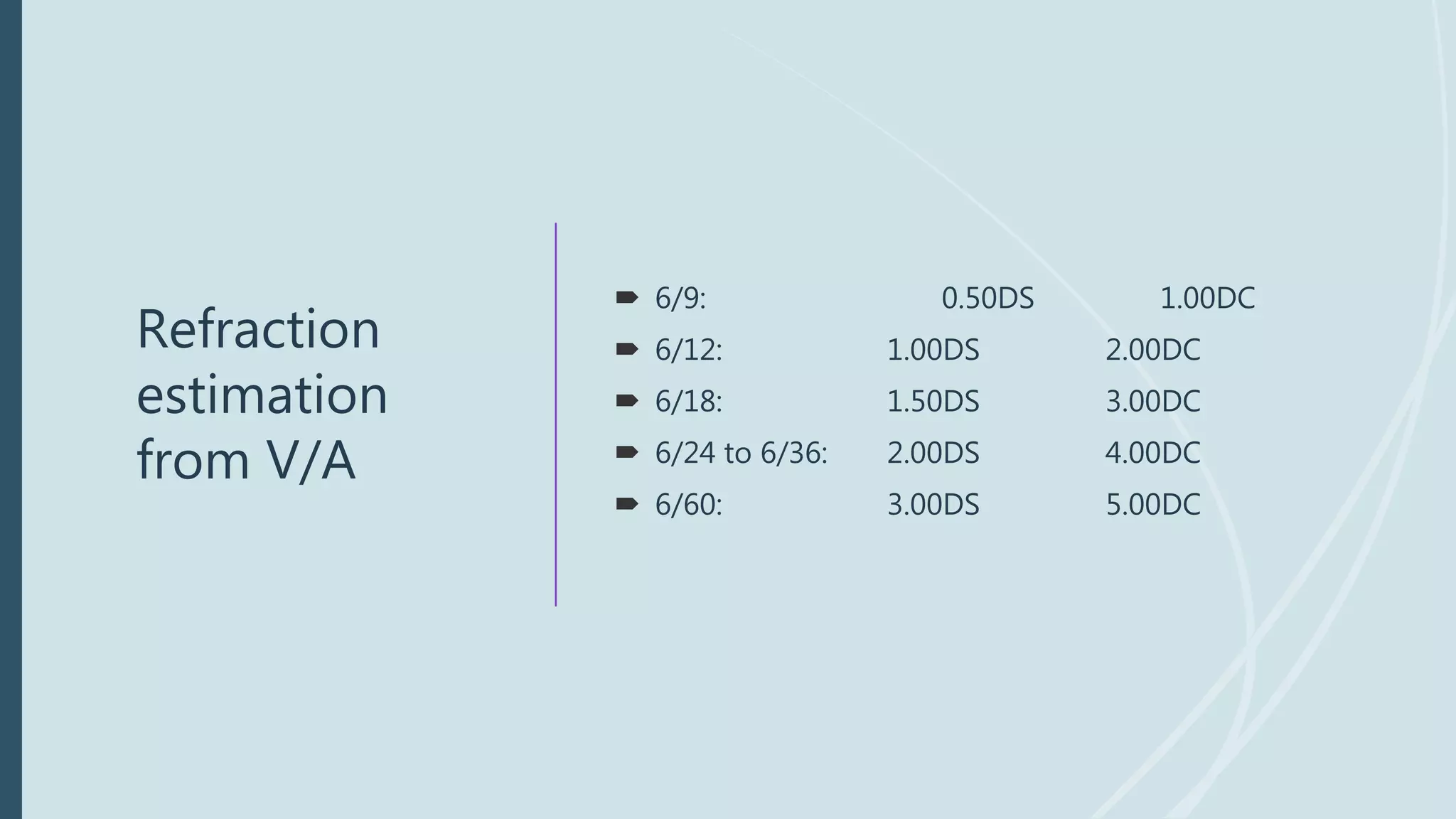
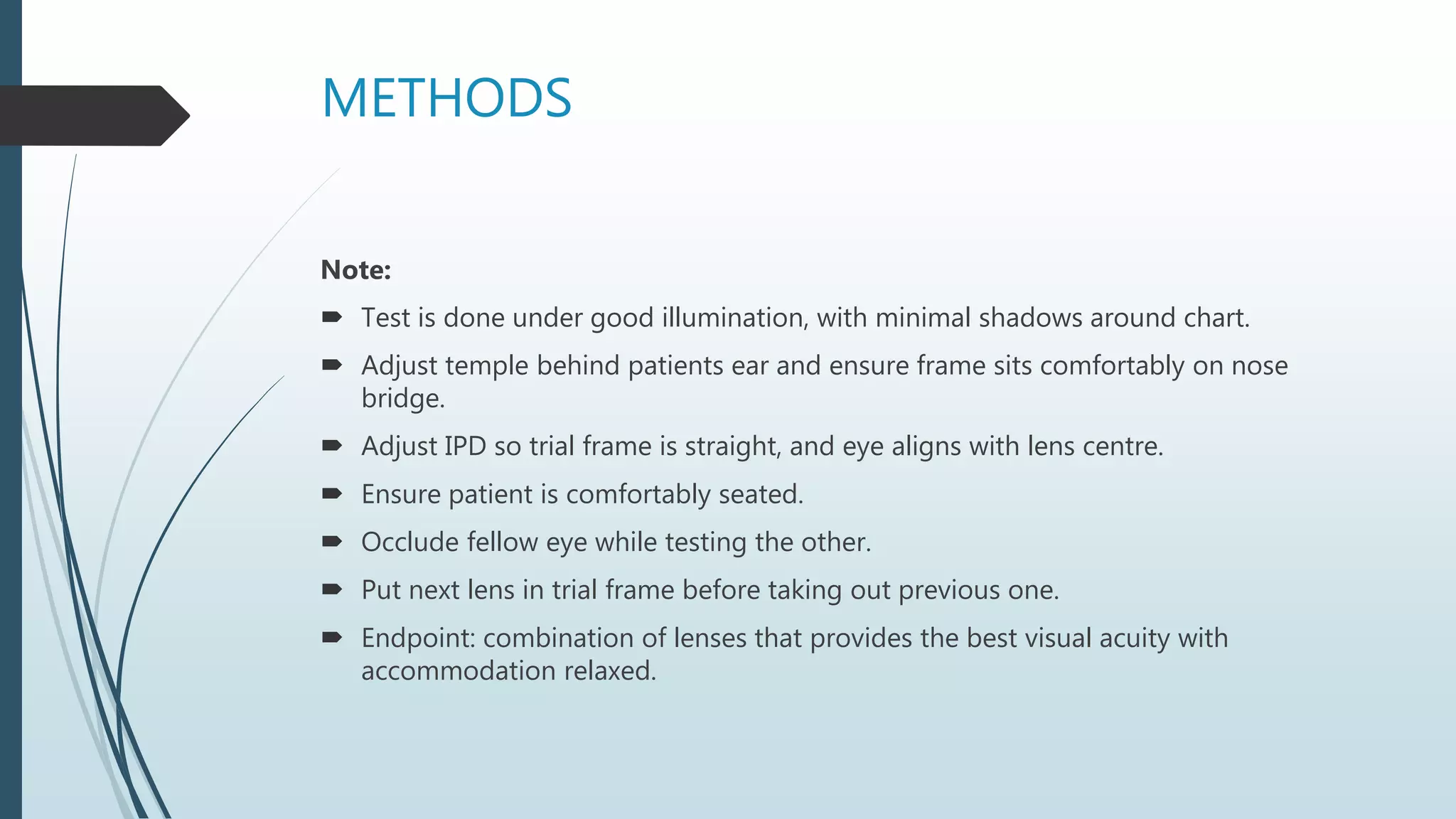
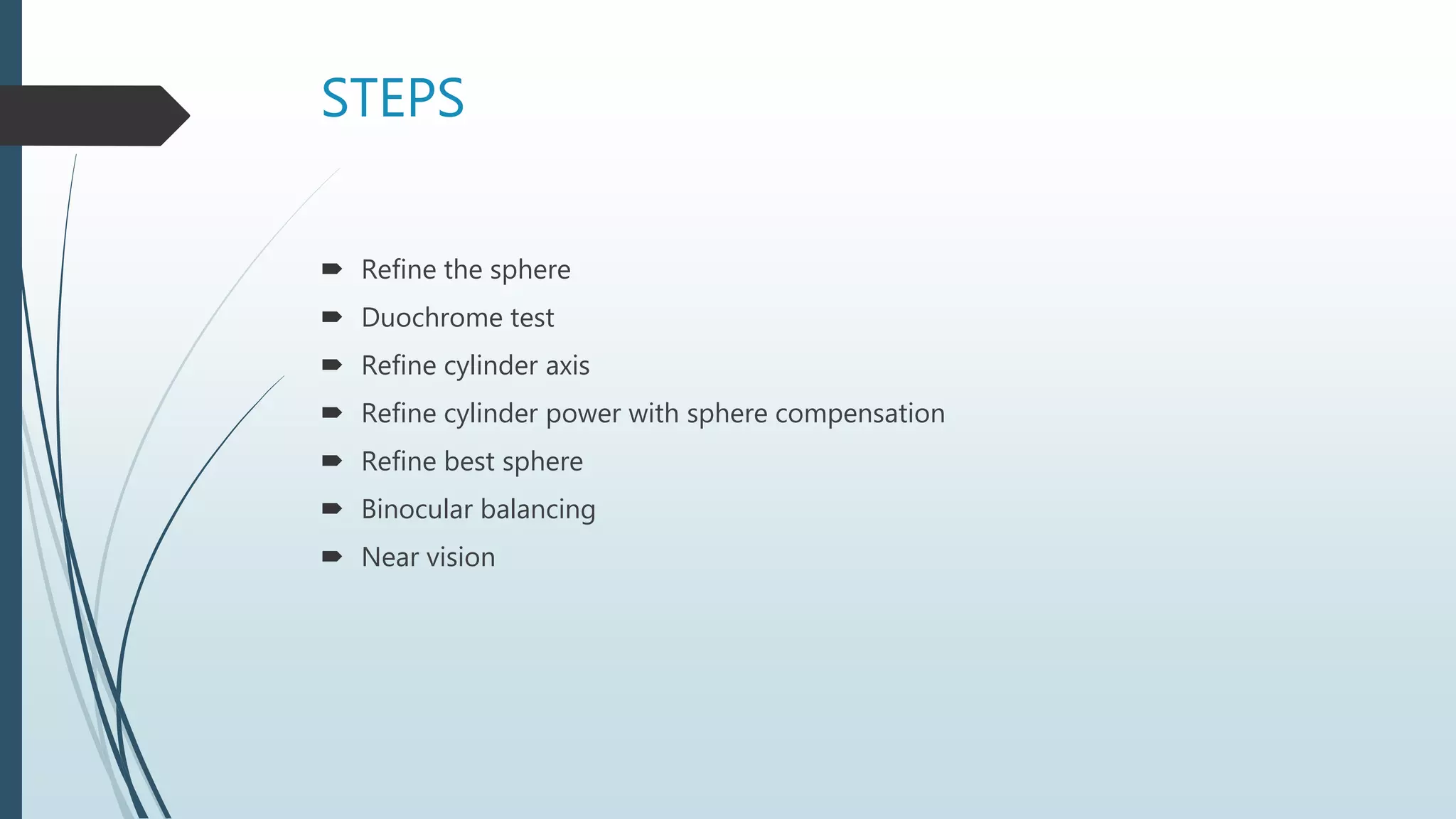
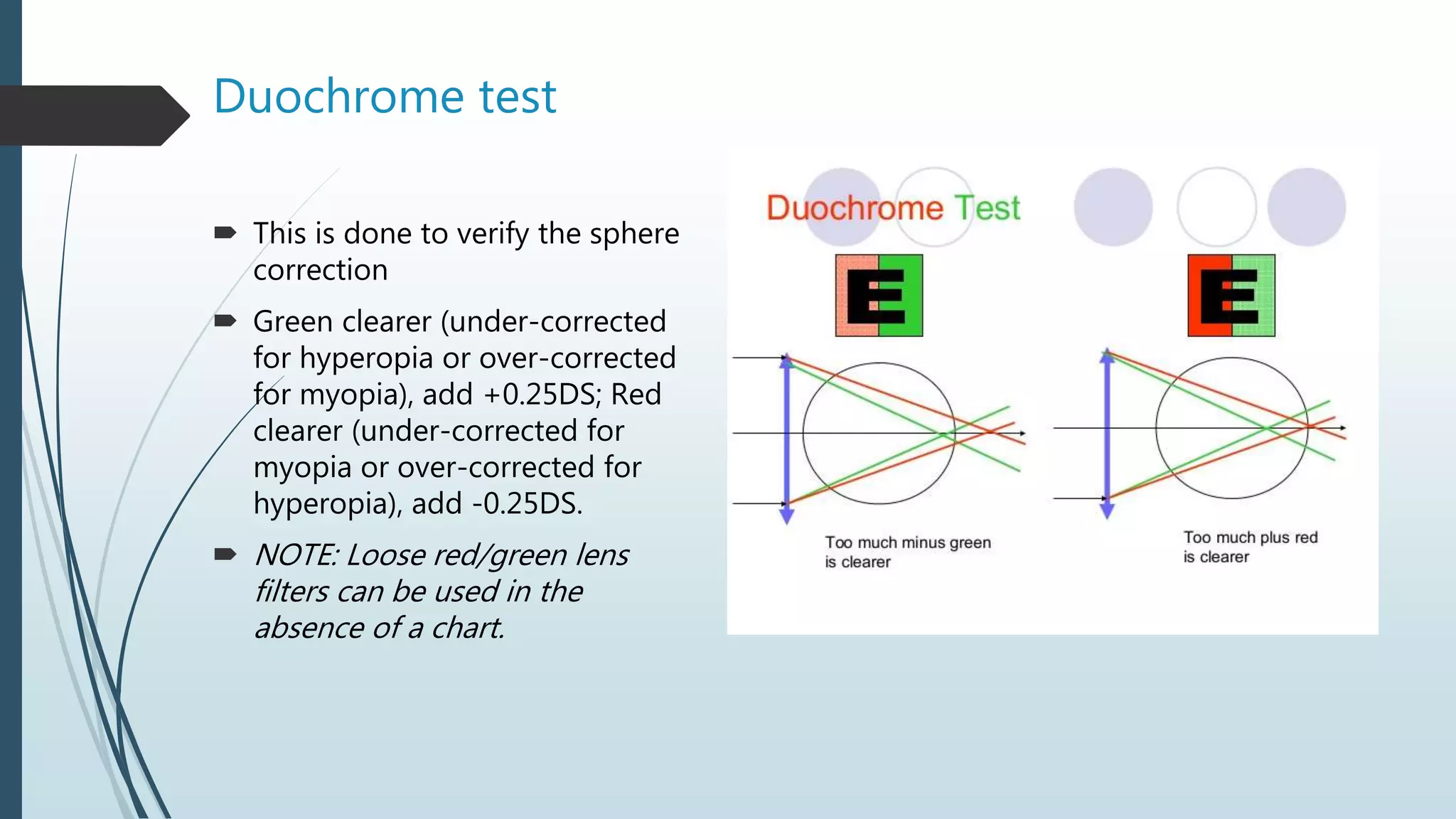
This document describes the methods and process of subjective refraction. Subjective refraction requires patient input to determine the best lens correction. The examiner uses trial lenses and frames along with visual acuity tests to refine the lens prescription through spherical, cylindrical, and axis adjustments until the best visual acuity is achieved. The process involves initially estimating the refractive error and starting point based on history and tests, then iteratively adjusting lenses based on patient feedback to get the optimal prescription.