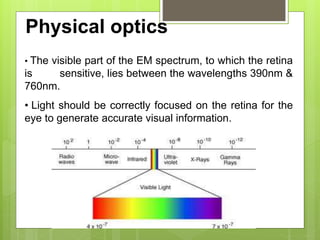
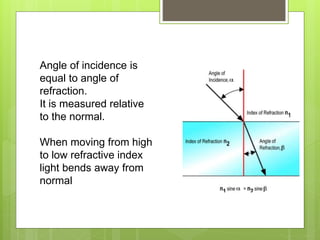
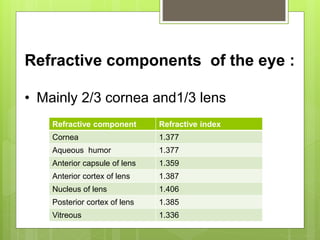
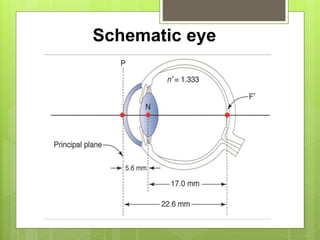
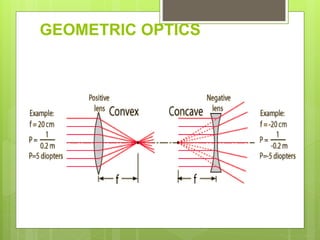
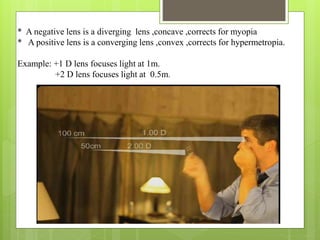
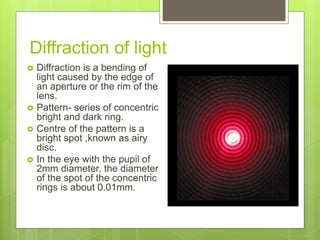
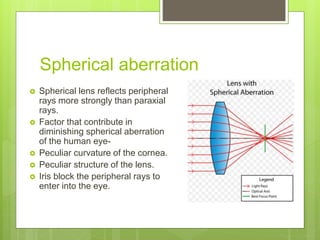
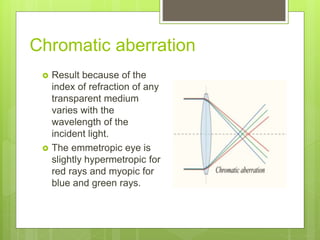
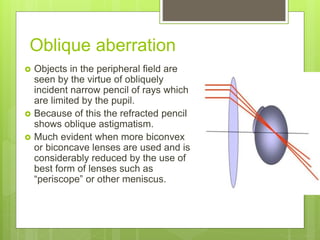
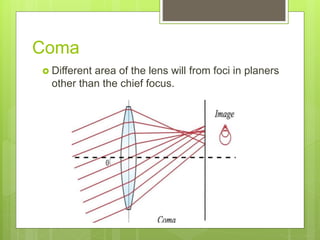
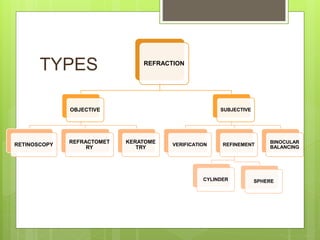
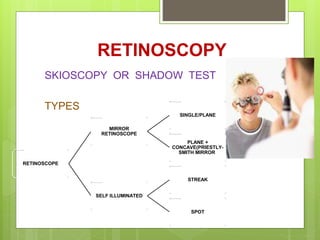
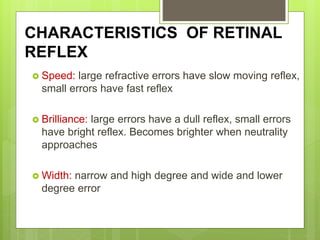
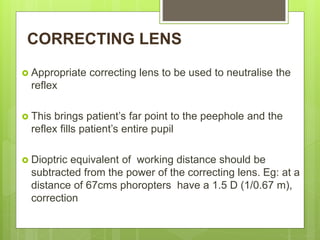
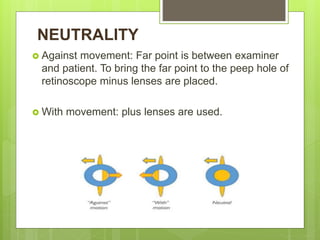
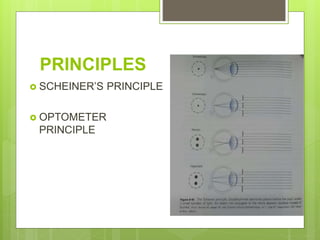
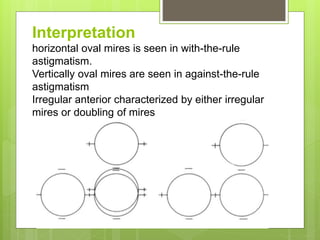
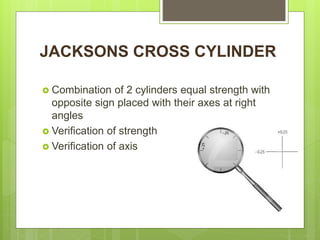
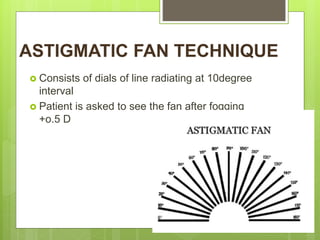
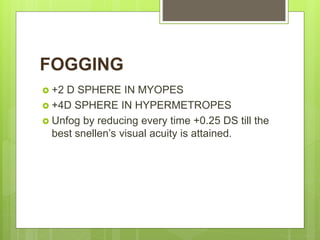
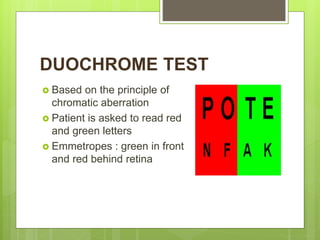
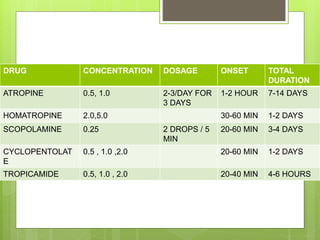
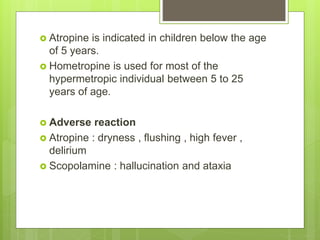
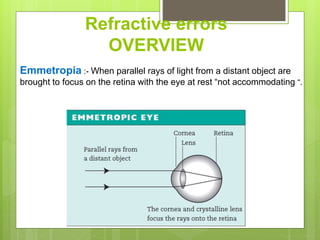
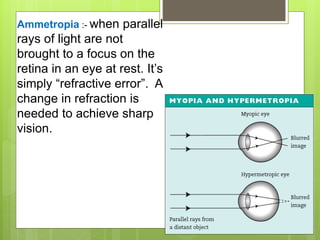
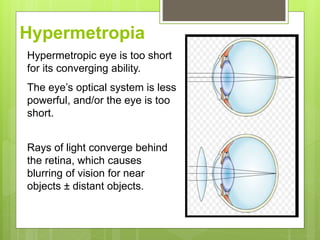
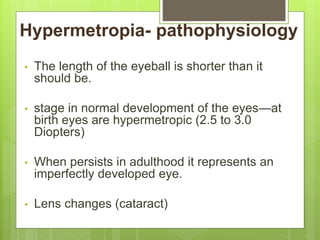
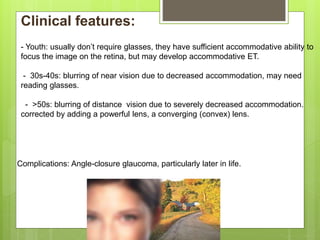
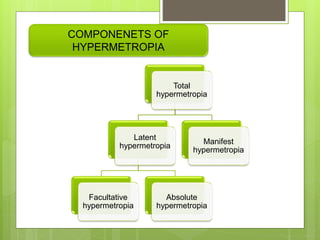
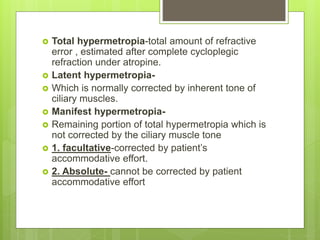
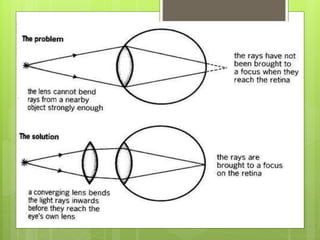
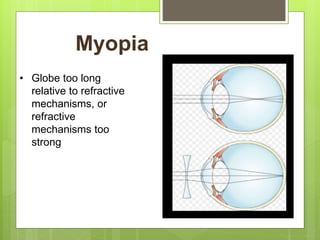
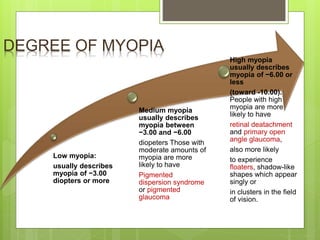
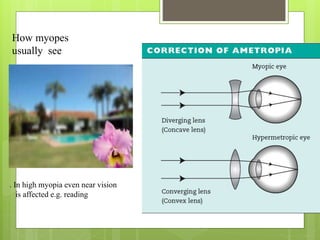
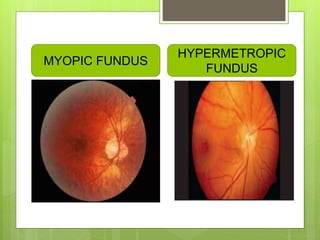
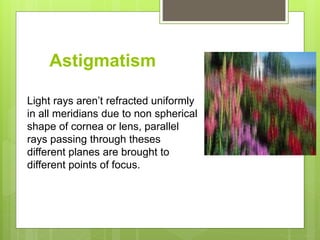
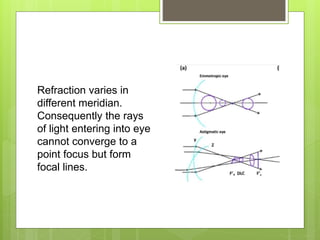
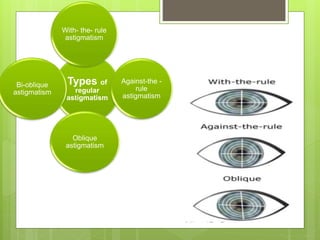
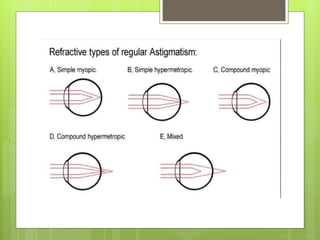
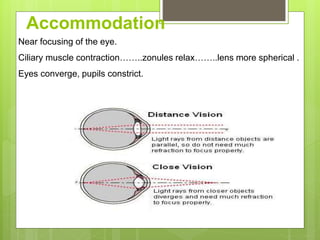
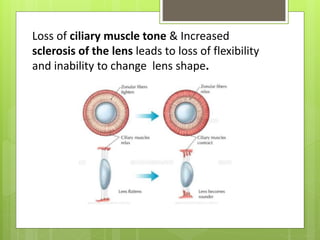
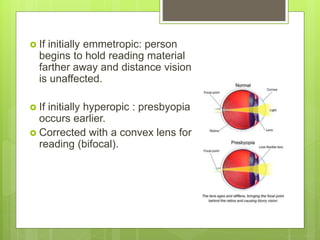
The document provides an overview of the principles of refraction and the structure and function of the eye. It details various types of refractive errors, including myopia, hyperopia, and astigmatism, along with methods for determining and correcting these errors through techniques such as retinoscopy and refractometry. The document also discusses optical aberrations, the anatomy of the eye, and the clinical implications of refractive conditions.