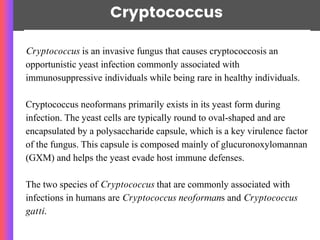
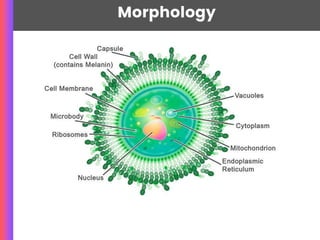
Cryptococcus is an invasive fungus that primarily causes cryptococcosis, particularly in immunocompromised individuals, and is characterized by a virulence-associated polysaccharide capsule. It can lead to severe infections such as cryptococcal meningitis and disseminated disease, often originating from inhaled spores found in soil and bird droppings. Diagnosis involves various methods including culture, antigen detection, and molecular techniques, while treatment may include antifungal medications like amphotericin B and triazoles.