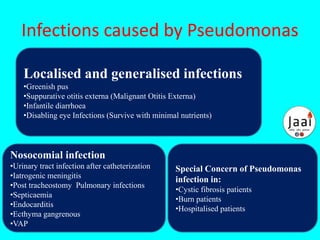
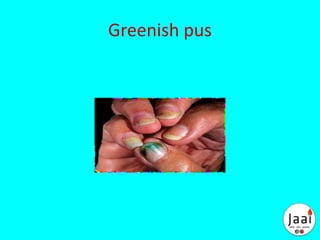
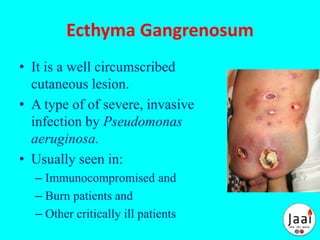
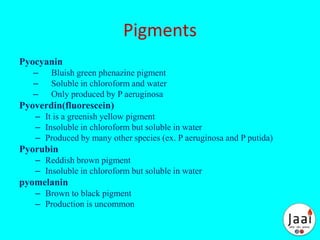
Pseudomonas are aerobic, non-spore forming, gram-negative bacilli that can cause opportunistic infections in humans and other hosts. Pseudomonas aeruginosa is a common cause of nosocomial infections and can infect the urinary tract, lungs, blood, and other sites. It is resistant to many antibiotics but can be treated with combinations including gentamicin and carbenicillin. Pseudomonas produces pigments like pyocyanin and pyoverdin and secretes toxins and enzymes that contribute to its virulence and ability to infect compromised hosts like burn patients.