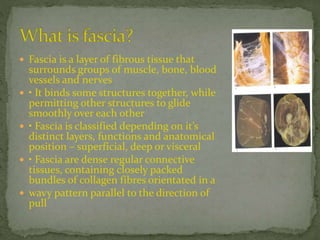
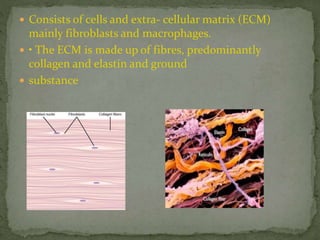
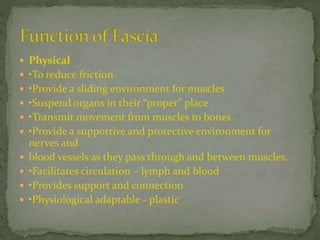
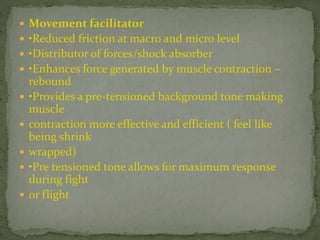
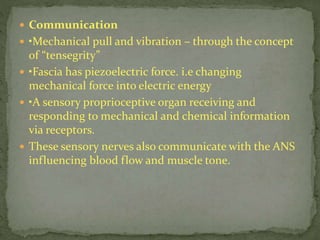
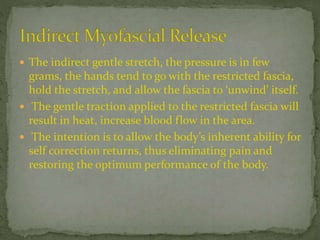
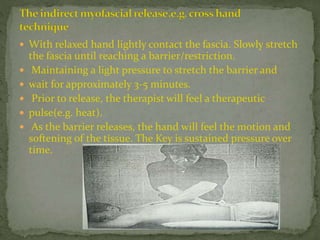
This document discusses myofascial pain syndrome (MPS), also known as chronic myofascial pain. MPS is characterized by chronic pain caused by multiple trigger points and fascial constrictions. Fascia is a layer of fibrous tissue that surrounds muscles, bones, blood vessels and nerves. Trigger points in fascia can cause focal tenderness and referred pain patterns. Myofascial release techniques aim to relax contracted muscles and stimulate the stretch reflex by applying sustained pressure to fascial restrictions to allow the tissue to elongate. MPS is a common cause of chronic pain that can be treated through myofascial release.
![ Fibroscitis [Sir.William Goyers]
Myofascitis [Albee]
Nonarticular rhuematism
Tension myalgia
MPS are among the most commonly
overlooked causes of chronic pain and
disability in medicine (Simons 1988).
Travell described the term “Trigger point’ and
adopted the expression Myofascial pain
syndrome.“ fibrositis” myofascial pain
syndrome+ fibromyalgia](https://image.slidesharecdn.com/mayofacialreleasetechnique-200420110245/85/Mayofacial-release-technique-2-320.jpg)