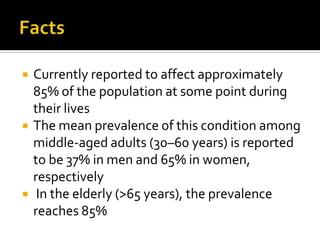
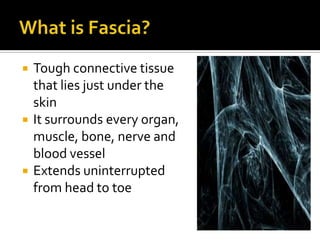
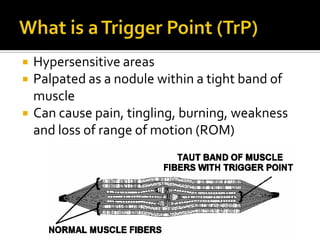
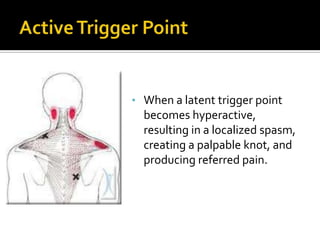
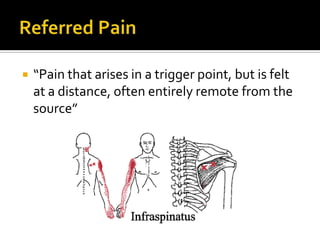
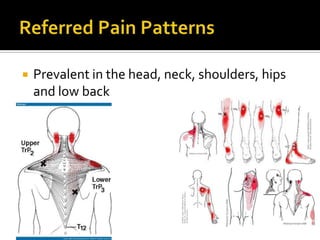
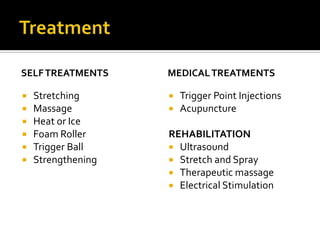
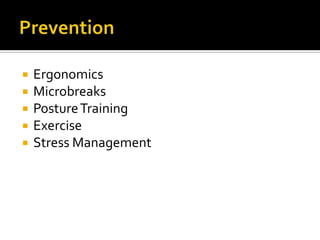
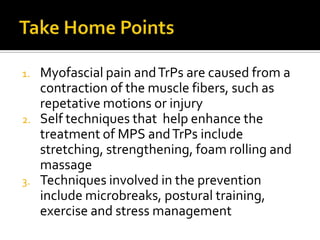
This document discusses myofascial pain and trigger points (TrPs). It defines myofascial pain as pain caused by hypersensitive areas in the fascia surrounding muscles that can cause referred pain. Trigger points are identified as localized knots within tightened bands of muscle that produce referred pain. The document provides information on causes, symptoms, diagnosis, treatment techniques for myofascial pain such as stretching, massage, and trigger point injections, as well as guidelines for prevention.