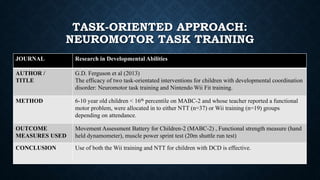
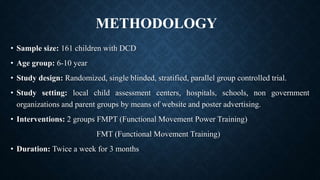
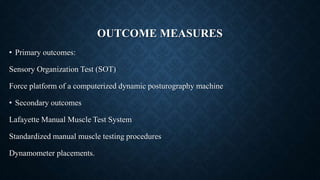
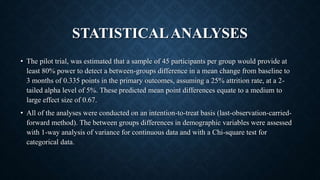
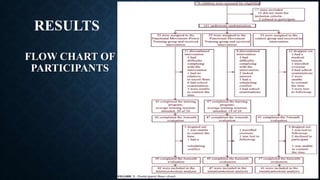
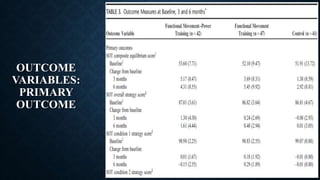
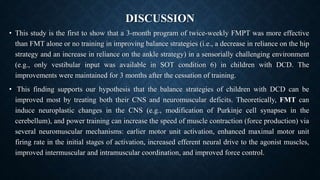
The study compared the effectiveness of two novel balance training programs (Functional Movement-Power Training and Functional Movement Training) to no training in children with Developmental Coordination Disorder. 161 children were randomly assigned to one of the three groups and underwent their respective interventions twice a week for 3 months. Outcome measures of balance strategies and neuromuscular performance were taken before and after the intervention period using computerized dynamic posturography and manual muscle testing. The results showed that both novel training programs improved balance and strength to a greater extent than no training.


![JOURNAL Physical Therapy
AUTHOR /
TITLE
Leandra Gonsalves et al (2015).
Children with developmental coordination disorder play active virtual reality games differently than
children with typical development.
METHOD 21 children with DCD of age group 10-12 year and typically developing children played a match of
table tennis on each AVG type.
MODALITY Linear mixed model analyses – Move and Kinect AVG type for forehand and back hands
CONCLUSION If a therapeutic goal o]is to promote movement quality in children with DCD, clinical judgement is
required to select the most appropriate AVG and determine whether movement quality is adequate for
unsupervised practice
ACTIVE VIRTUAL GAMING](https://image.slidesharecdn.com/jp2-200918100845/85/Developmental-Co-ordination-Disorder-DCD-Physiotherapy-management-23-320.jpg)