The document discusses mandibular fractures, including:
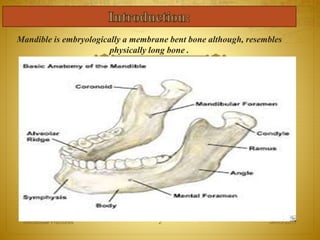
1. The mandible is the strongest bone in the face and resembles a long bone in structure.
2. Mandibular fractures are commonly caused by vehicular accidents, assaults, falls, and sports or work injuries.
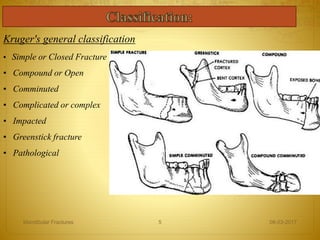
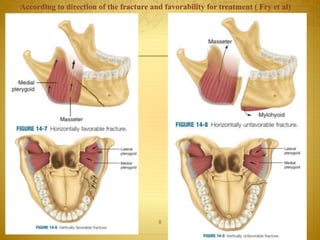
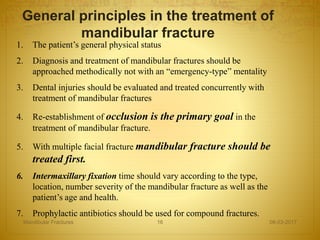
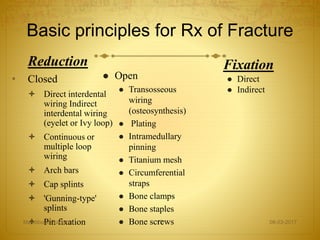
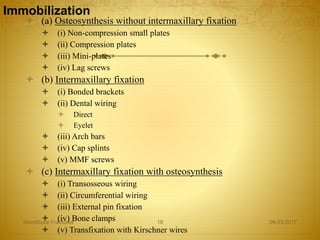
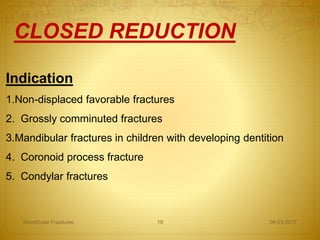
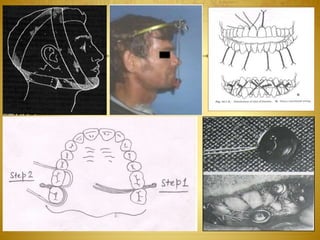
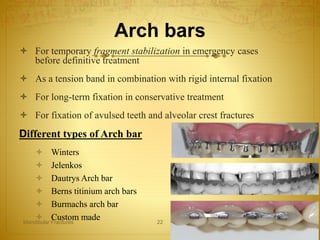
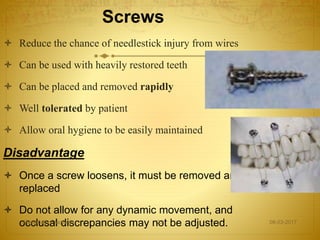
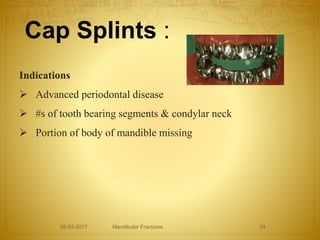
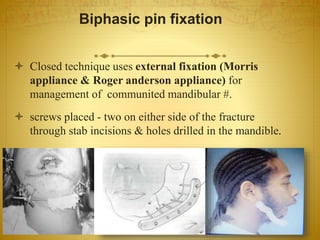
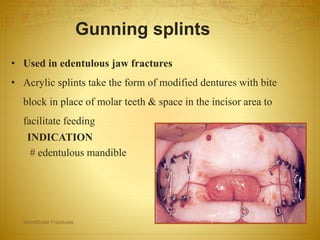
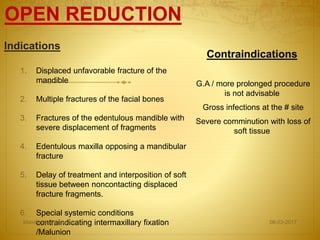
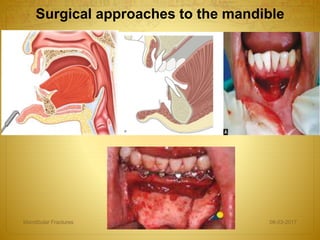
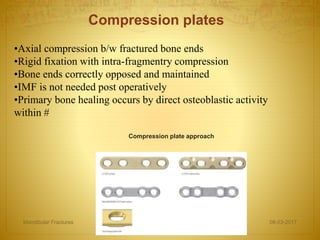
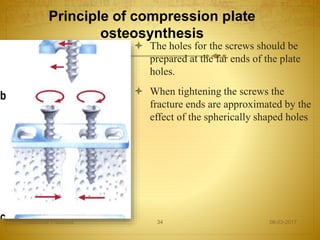
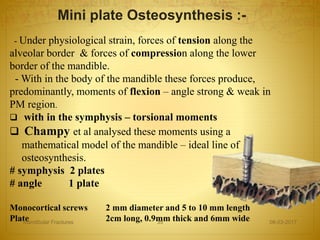
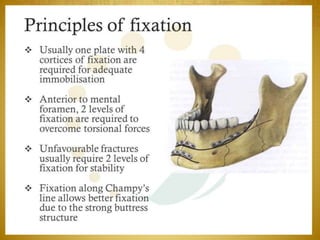
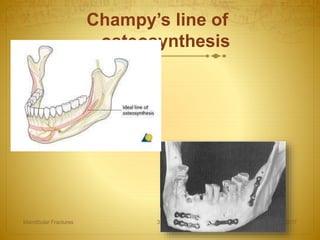
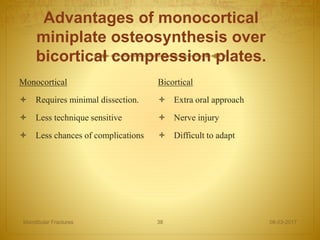
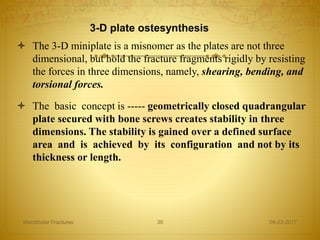
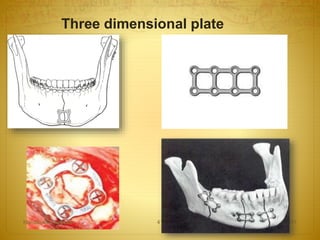
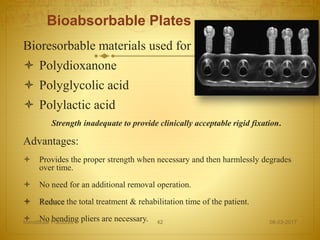
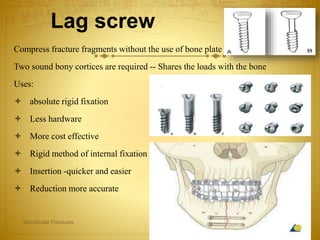
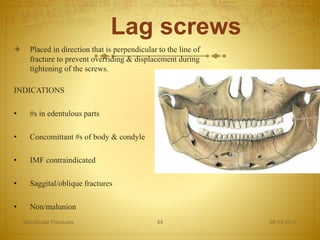
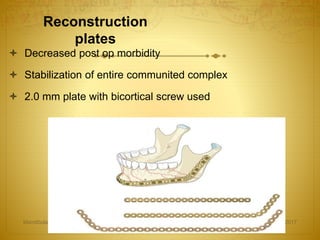
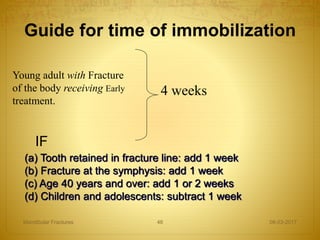
3. Treatment involves either closed or open reduction methods depending on the type and severity of the fracture. Open reduction using mini plates placed along Champy's line of osteosynthesis allows for rigid internal fixation without intermaxillary fixation.