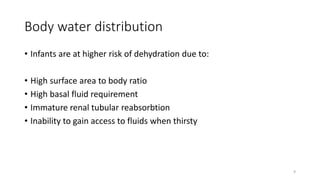
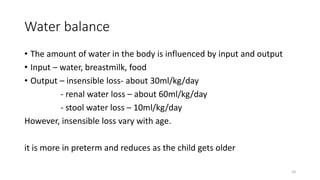
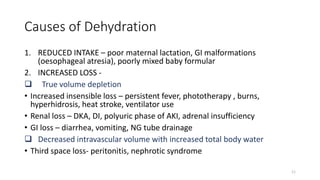
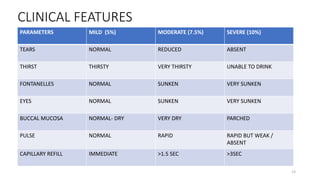
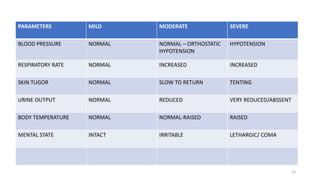
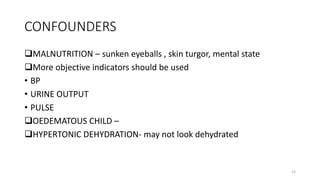
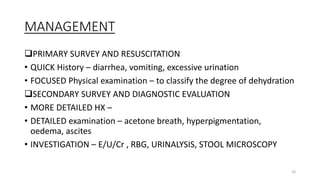
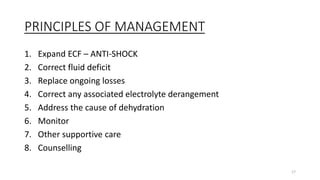
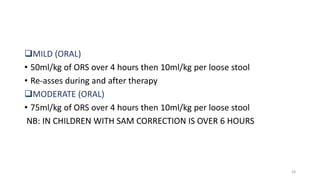
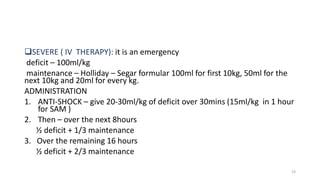
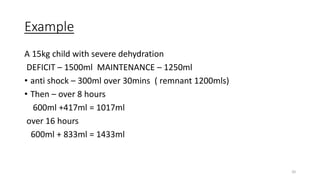
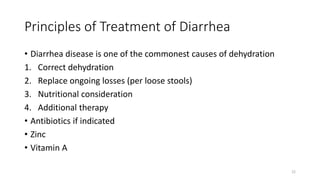
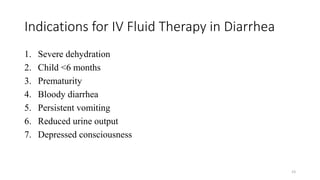
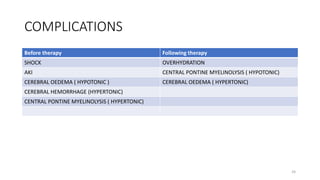
This document presents a case study of a 7-month-old girl with severe dehydration due to diarrhea and vomiting. The child shows several signs of severe dehydration including lethargy, depressed fontanelles, and capillary refill time over 4 seconds. Severe dehydration is estimated at over 10% body weight loss. Management of severe dehydration involves rapid intravenous rehydration to replace fluid deficit and ongoing losses, followed by monitoring for complications like overhydration or electrolyte imbalances. Proper treatment of dehydration is important to reduce morbidity and mortality in infants and children.