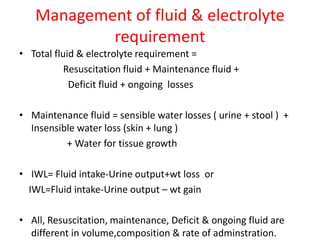
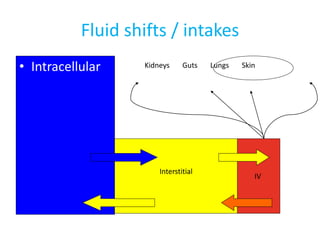
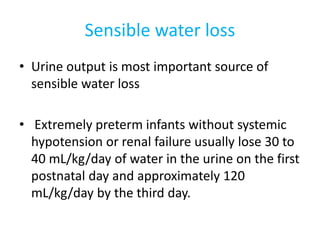
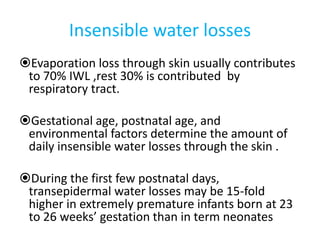
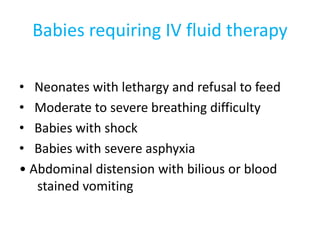
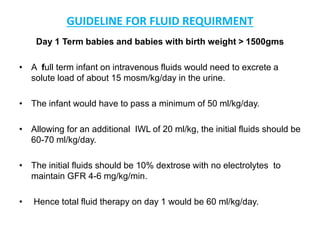
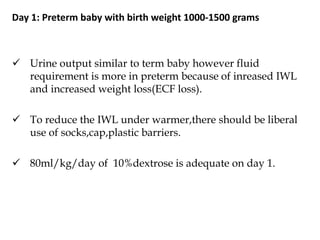
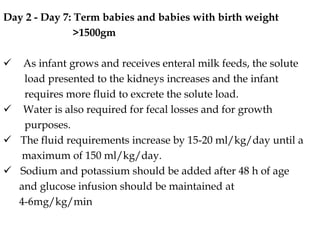
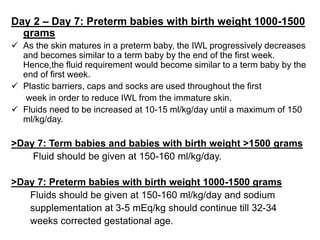
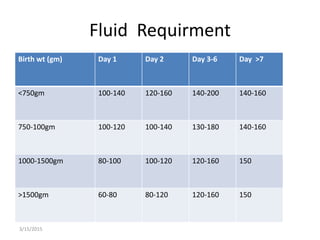
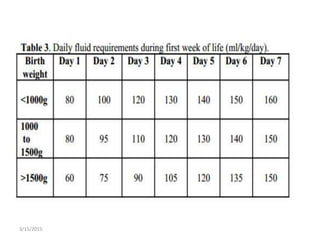
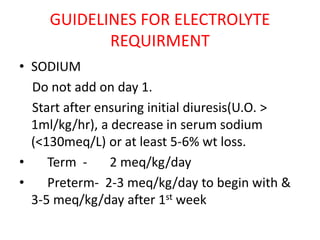
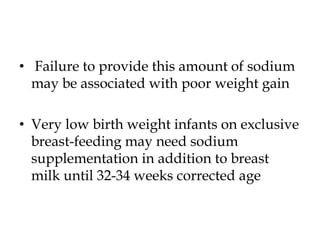
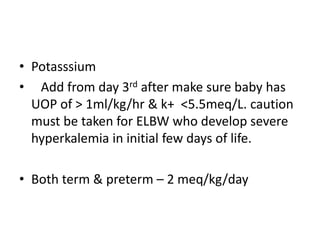
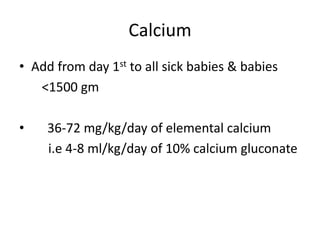
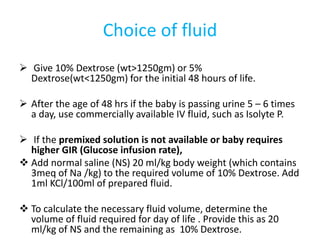
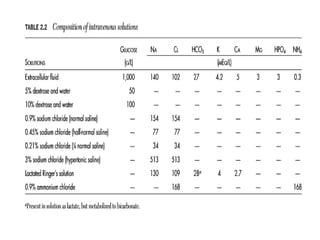
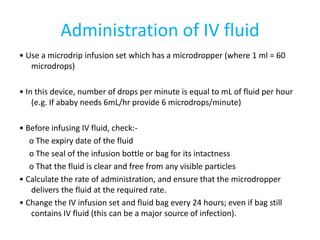
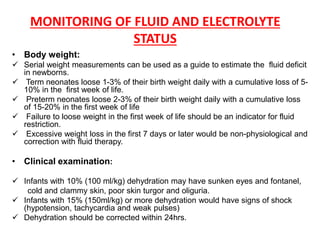
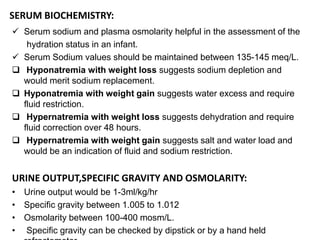
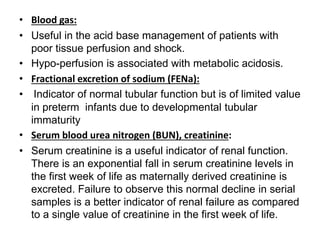
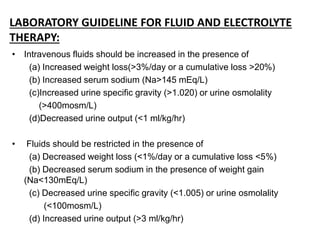
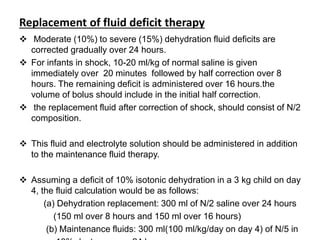
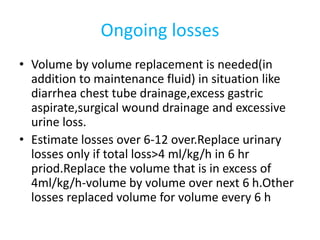
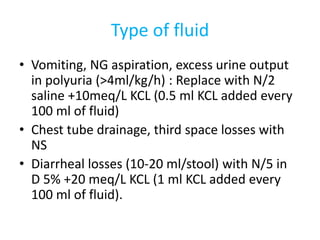
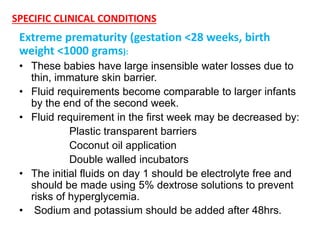
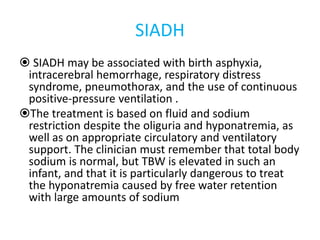
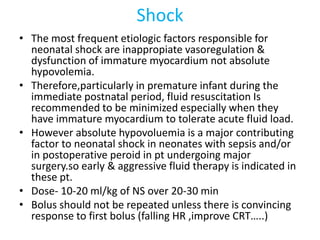
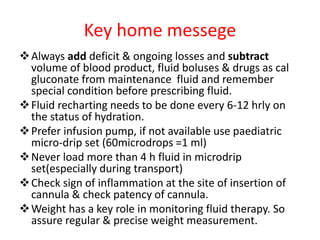
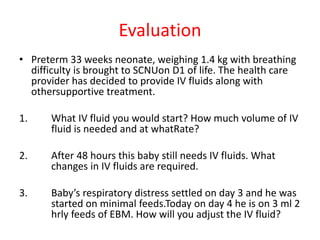
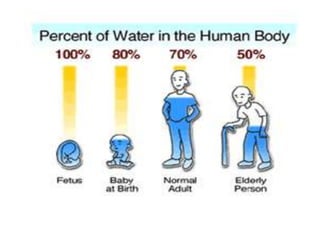
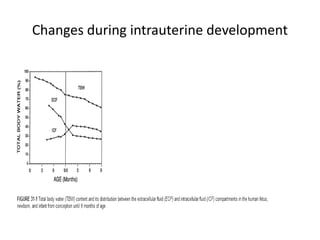
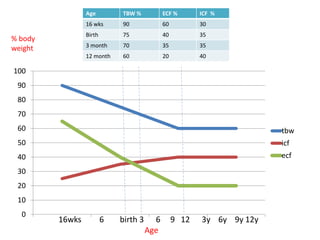
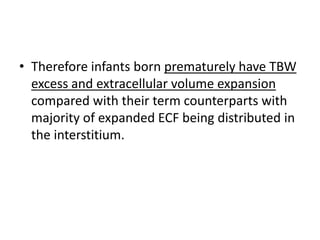
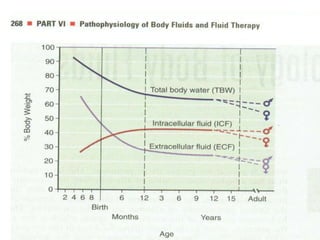
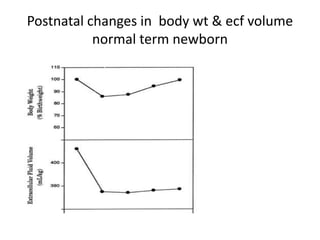
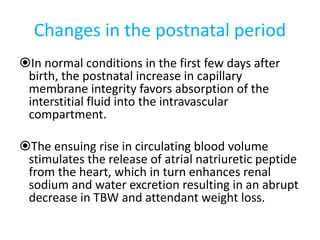
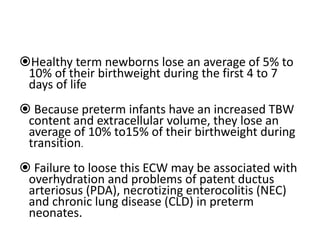
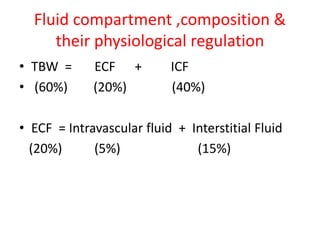
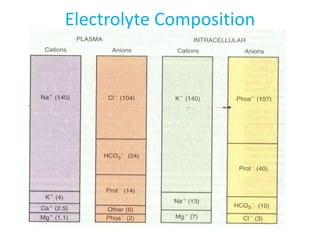
This document provides an overview of neonatal fluid and electrolyte requirements, including physiological changes affecting balance in fetuses and neonates. It discusses developmental changes in total body water, extracellular and intracellular fluid during gestation and after birth. Maturation of organs like the cardiovascular system and kidneys that regulate fluid compartments is also covered. Guidelines are provided for calculating total fluid needs as well as maintenance, deficit and ongoing loss replacement in both term and preterm infants of different weights. Electrolyte supplementation amounts and choices of IV fluids are also summarized.



![Osmolality
• Calculated osmolality
2 [Na+] + [Glucose] /18 + [BUN]/2.8
• Effective osmolality /Tonicitiy
2[Na+] + [Glucose]/18
• Measured Osmolality –measured by degree of
freezing point depression](https://image.slidesharecdn.com/newfluid-150315094706-conversion-gate01/85/Neonatal-fluid-requirements-and-specials-conditions-22-320.jpg)