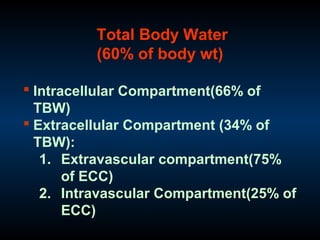
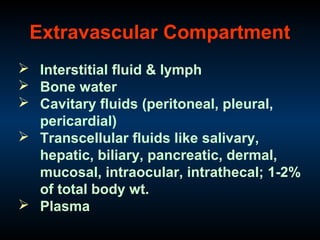
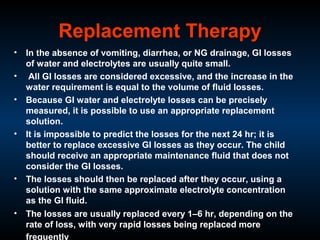
This document discusses fluids in the human body. It covers topics such as total body water, intracellular and extracellular fluid compartments, fluid intake and output, and perioperative fluid management. Specifically, it addresses maintenance fluid therapy, calculating fluid requirements based on weight, and replacing preoperative deficits and ongoing losses through replacement therapy. Replacement solutions are discussed for various fluid losses through the gastrointestinal tract, urine, drains, and third spacing.