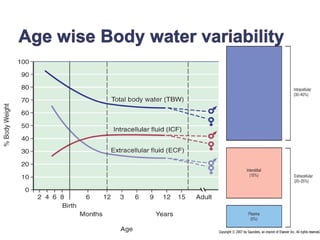
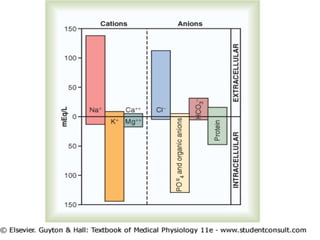
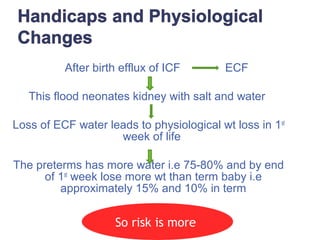
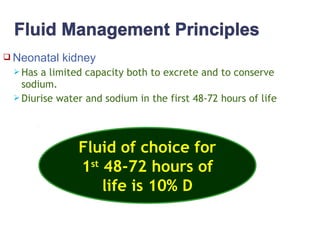
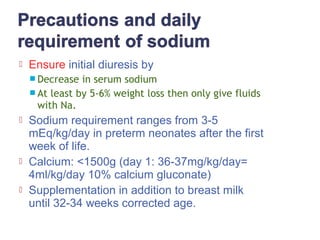
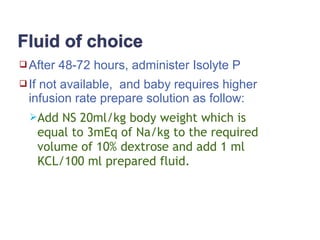
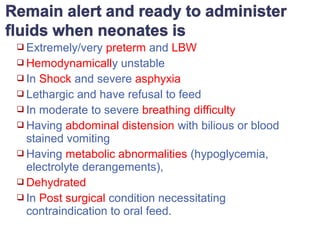
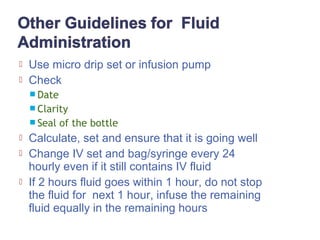
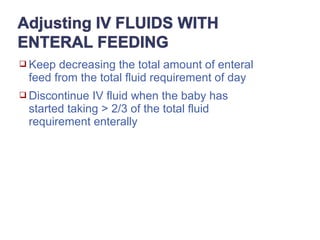
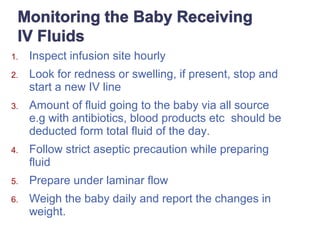
This document discusses fluid and electrolyte management in neonates. It outlines the physiological changes in neonates that impact fluid needs, including higher total body water and immature kidney function. It provides guidelines for calculating daily fluid requirements based on gestational age and weight. It describes the use of IV fluids for initial resuscitation and maintenance, adjusting for enteral feedings and weight changes. Conditions requiring IV fluids and formulas for replacing various fluid losses are also summarized.





















![1. Murat I, Humblot A, Girault L, Piana F. Neonatal fluid management. Best Pract Res Clin
Anaesthesiol. 2010 Sep;24(3):365–74.
2. Chawla D, Agarwal R, Deorari AK, Paul VK. Fluid and electrolyte management in term and preterm
neonates. Indian J Pediatr. 2008 Mar 1;75(3):255.
3. Jalan Anup. Practical approach to fulid and electrolyte management in newborns. In: Advances in
pediatrics. 2nd ed. JP Medical Ltd; p. 16–23.
4. Fluid and electrolyte management in term and preterm neonates | SpringerLink [Internet]. [cited 2017
Dec 12]. Available from: https://link.springer.com/article/10.1007/s12098-008-0055-0
5. Fluid and Electrolyte Management in the Newborn [Internet]. University of Iowa Children’s Hospital.
2012 [cited 2017 Dec 12]. Available from: https://uichildrens.org/health-library/fluid-and-electrolyte-
management-newborn
6. Fluid, Electrolyte, and Nutrition Management of the Newborn: Overview, Prevalence and Loss of
Body Water, Assessing Fluid and Electrolyte Status. 2017 May 2 [cited 2017 Dec 12]; Available
from: https://emedicine.medscape.com/article/976386-overvie
7. Lonnqvist PA. Fluid management in association with neonatal surgery: even tiny guys need their
salt. British Journal of Anaesthesia, Volume 112, Issue 3, 1 March 2014, Pages 404–
406, https://doi.org/10.1093/bja/aet436
8. Ciccarelli S, Stolfi I, Caramia G. Management strategies in the treatment of neonatal and pediatric
gastroenteritis. Infect Drug Resist. 2013 Oct 29;6:133–61.
9. NNT, UNICEF. Participant Manual- Faclilty Based Care of Sick Neonate at Referral Health Facility.
Pg: 41-43. In.](https://image.slidesharecdn.com/fluidmanagementoflbwgeetanjli-171220070813/85/Fluid-and-electrolyte-management-among-neonates-35-320.jpg)
