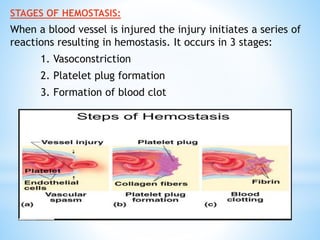
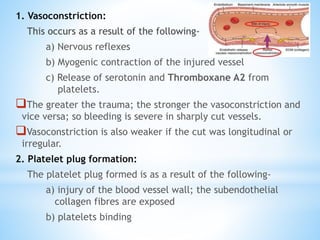
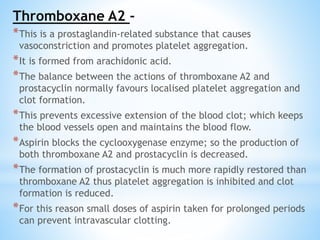
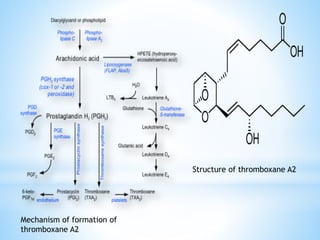
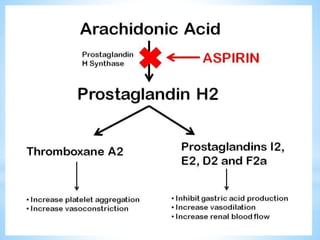
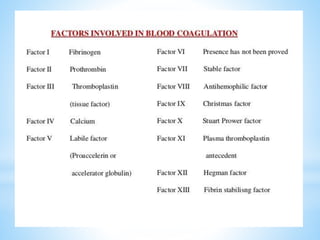
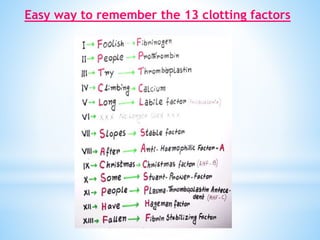
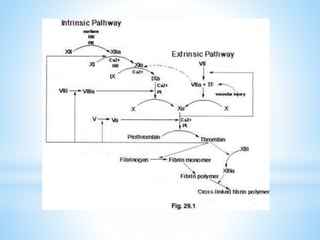
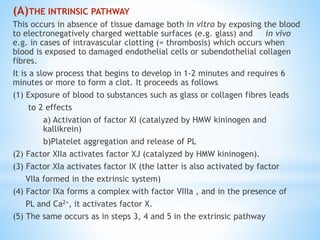
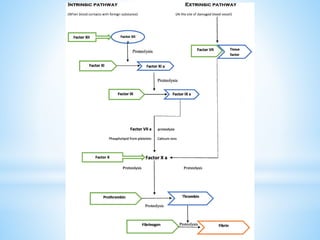
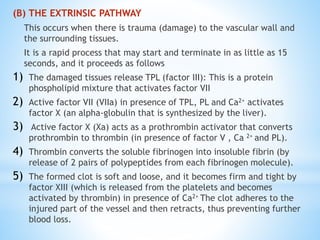
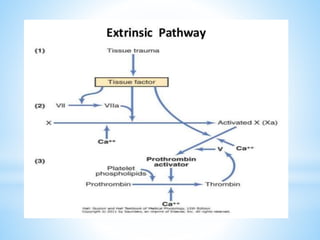
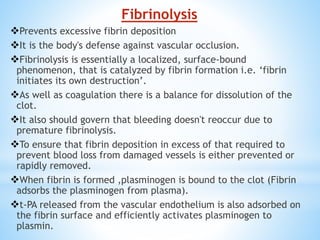
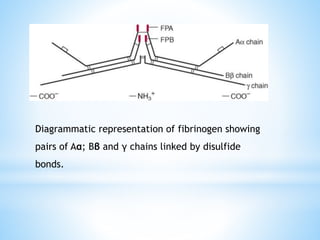
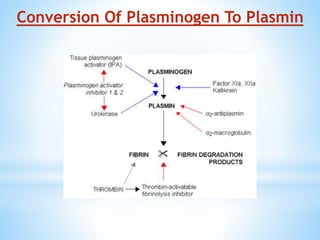
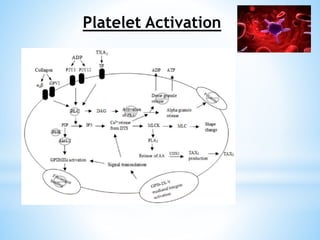
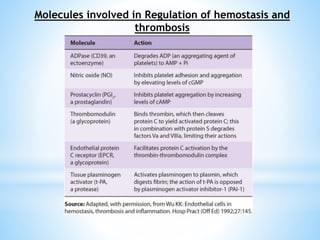
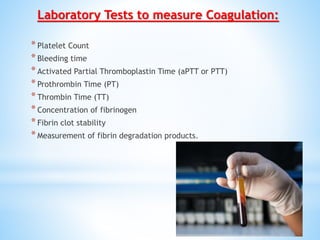
This document summarizes the process of hemostasis and coagulation. It begins with definitions of key terms like hemostasis, coagulation, and thrombosis. It then describes the three stages of hemostasis - vasoconstriction, platelet plug formation, and blood clot formation. The roles of platelets, thromboxane A2, and fibrin in coagulation are explained. Finally, it provides an overview of the intrinsic and extrinsic coagulation pathways and the role of calcium and vitamin K in blood clotting.