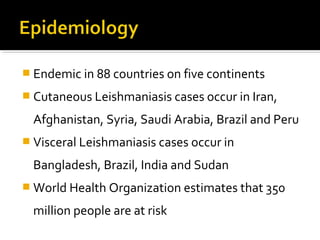
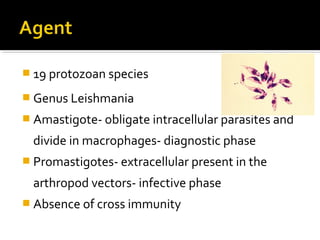
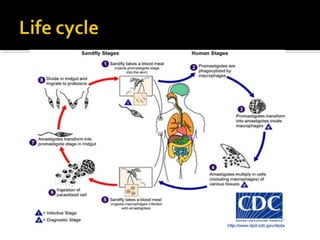
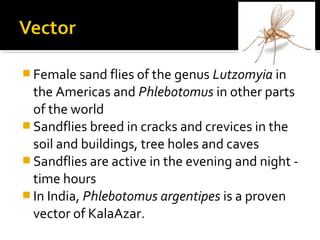
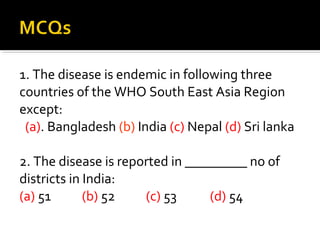
- Leishmaniasis is a protozoal disease caused by Leishmania parasites and transmitted by sandfly bites. It is endemic in 88 countries across 5 continents.
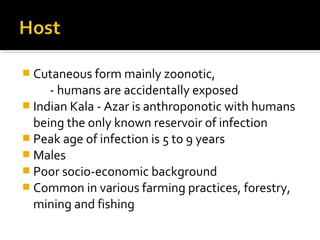
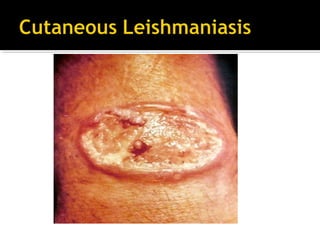
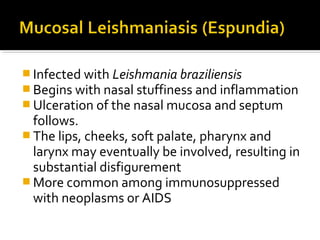
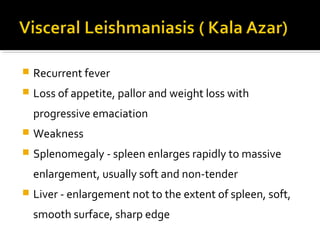
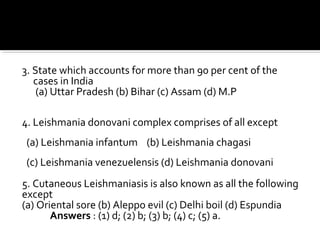
- There are several clinical forms including cutaneous, mucocutaneous, and visceral leishmaniasis. Visceral leishmaniasis, also known as kala-azar, is the most serious form and if left untreated is usually fatal.
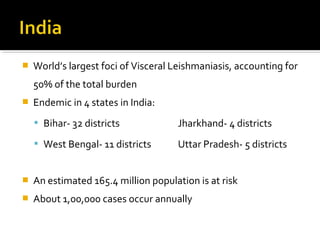
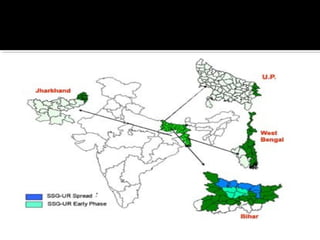
- India has the largest burden of visceral leishmaniasis worldwide, accounting for over half of global cases. It is endemic in 4 states, primarily Bihar where most cases occur.