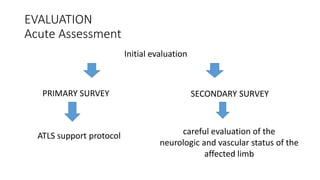
Traumatic knee dislocations are rare injuries that require careful evaluation and management. According to the document, knee dislocations often result from high-energy injuries like motor vehicle collisions or falls. A thorough examination is needed to assess vascular and neurological status. Imaging can identify associated fractures. While some stable injuries may be treated non-operatively, unstable injuries or those with ligament disruption typically require surgical reconstruction. Complications may include neurovascular injuries, infections, and long-term issues like osteoarthritis. Early surgical intervention within 3 weeks of injury may lead to better outcomes compared to delayed treatment.









![Routine Angiogram
• concept of a routine angiogram for all suspected knee dislocations has been
the matter of debate.
Currently,
Angiography
(routine computed tomographic angiography [CTA] or magnetic resonance
angiography [MRA] )
is recommended for patients demonstrating insufficient perfusion or any
asymmetry in physical examination](https://image.slidesharecdn.com/knee-160123132056/85/Knee-13-320.jpg)