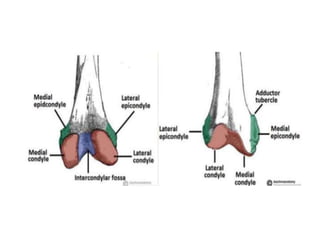
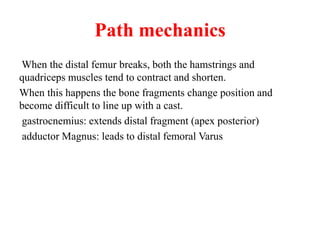
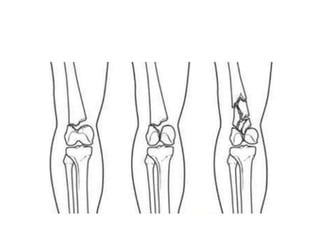
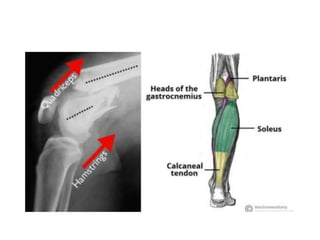
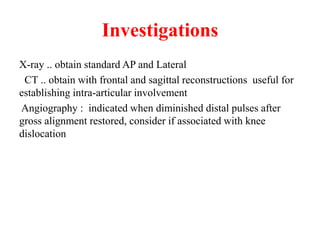
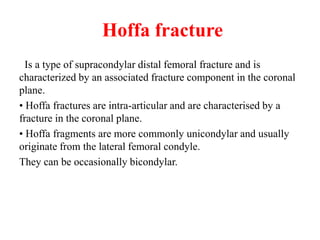
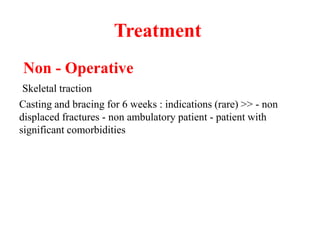
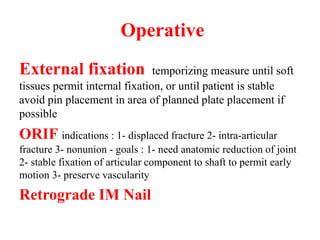
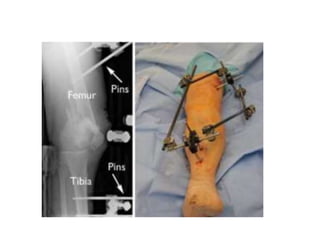
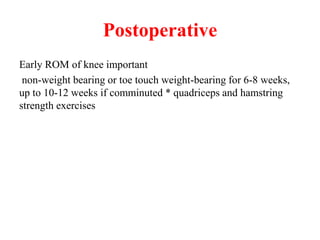
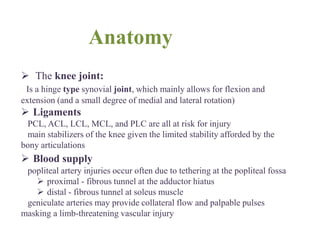
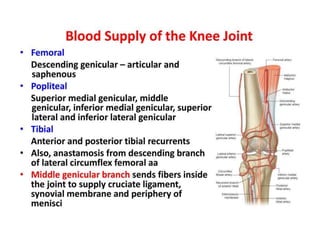
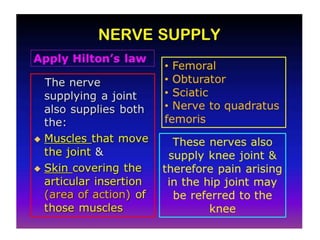
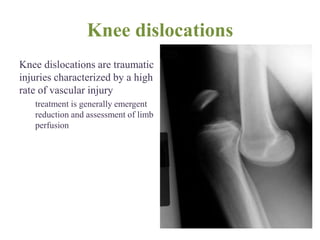
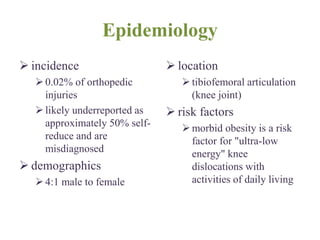
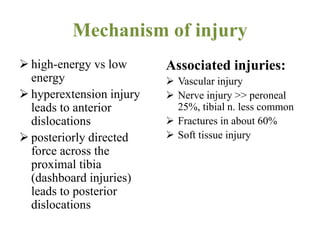
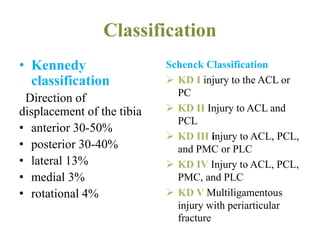
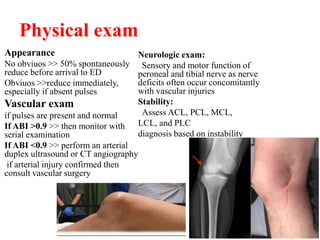
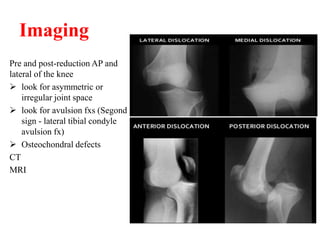
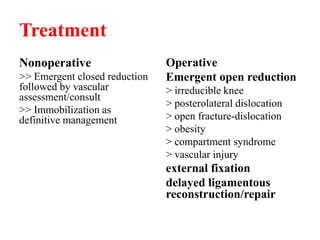
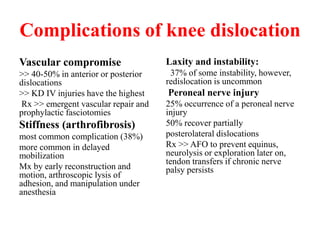
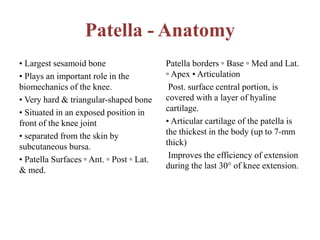
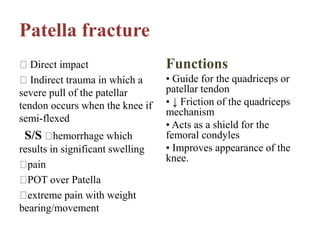
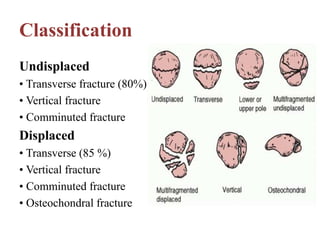
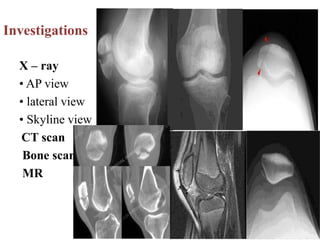
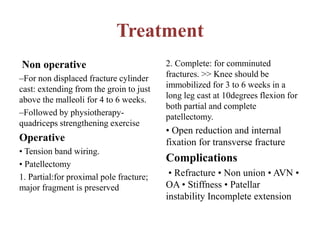
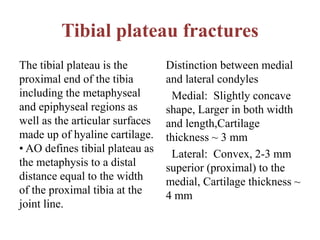
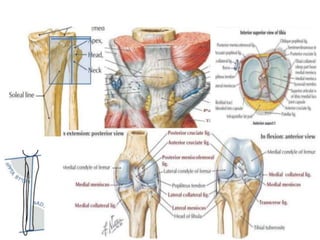
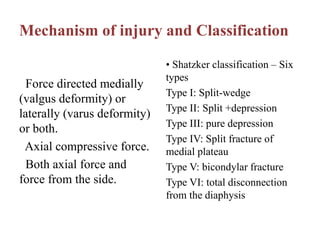
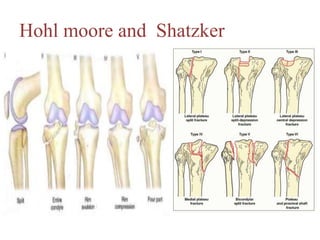
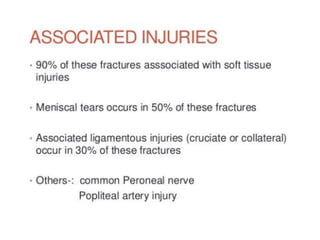
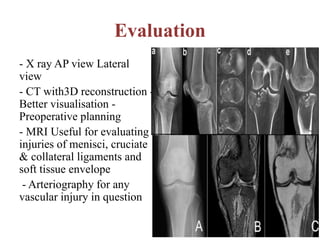
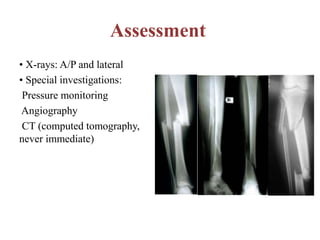
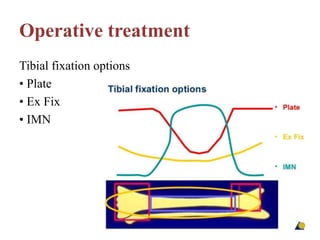
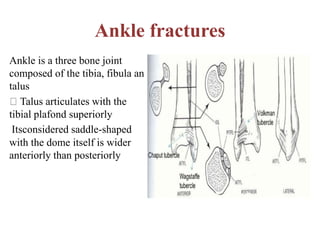
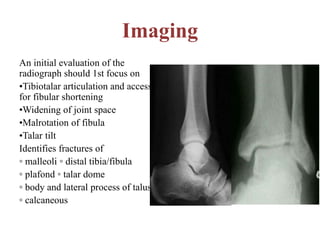
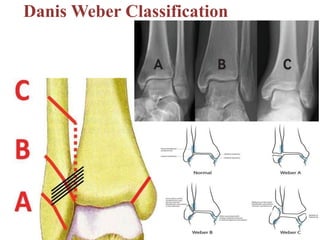
The document discusses various aspects of lower limb trauma, focusing primarily on distal femur fractures, knee dislocations, patella fractures, and tibial plateau fractures, including their definitions, anatomy, mechanisms of injury, classifications, and treatment options. It emphasizes the importance of accurate diagnosis through imaging and provides specific treatment protocols for both non-operative and operative management of these injuries. Additionally, it touches upon the complications associated with knee dislocations and other fractures, outlining essential rehabilitation strategies post-treatment.