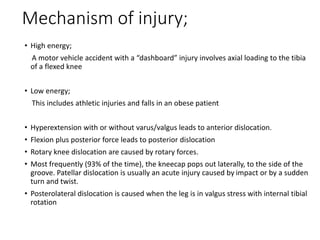
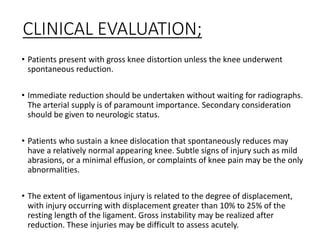
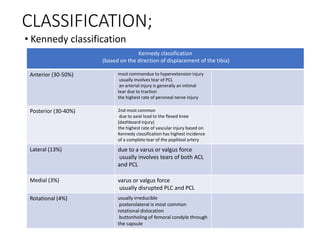
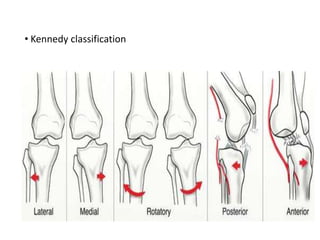
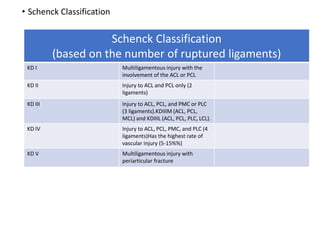
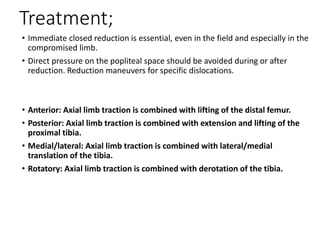
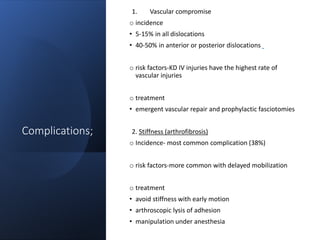
Knee dislocations are high-energy traumatic injuries that often involve ruptures of three or more major ligaments of the knee. They require emergent treatment due to the risk of neurovascular injury. The most common type is anterior dislocation from hyperextension. A thorough clinical exam is needed to assess ligament stability and neurovascular status before and after reduction. Vascular injury occurs in 20-60% of cases and requires revascularization within 8 hours to prevent limb loss. Immediate surgical exploration is indicated if pulses do not return after reduction.