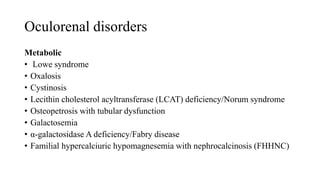
This document summarizes various ocular manifestations that can be associated with pediatric renal diseases. It discusses how the kidney and eye share developmental pathways and structural similarities. Several oculorenal disorders are described that involve malformations, ciliopathies, common structural defects, metabolic issues, phakomatoses, vascular diseases, and inflammation. Specific conditions like Bardet-Biedl syndrome, cystinosis, von Hippel-Lindau disease, and TINU are highlighted. Complications from corticosteroid therapy, end-stage renal disease, and renal dialysis that can impact the eye are also outlined.