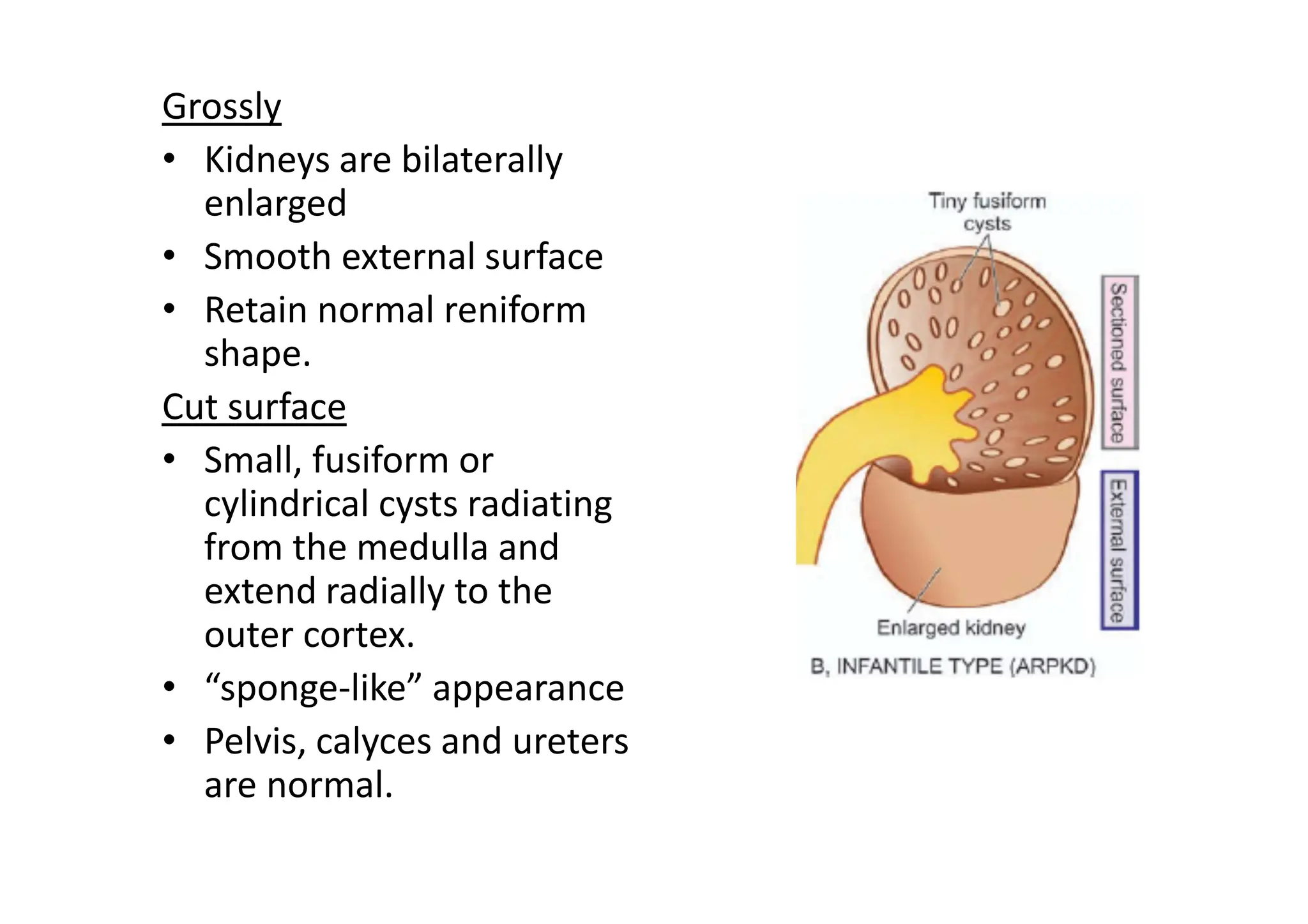
The document discusses kidney and lower urinary tract functions, including various diagnostic tests such as concentration and dilution tests, blood chemistry, and creatinine clearance tests. It categorizes kidney diseases into four major groups and details acute renal failure (ARF) and chronic renal failure (CRF), including their etiopathogenesis, clinical features, and the progression of symptoms. Additionally, it covers congenital malformations and cystic kidney diseases, specifically focusing on adult and infantile polycystic kidney disease and their clinical implications.