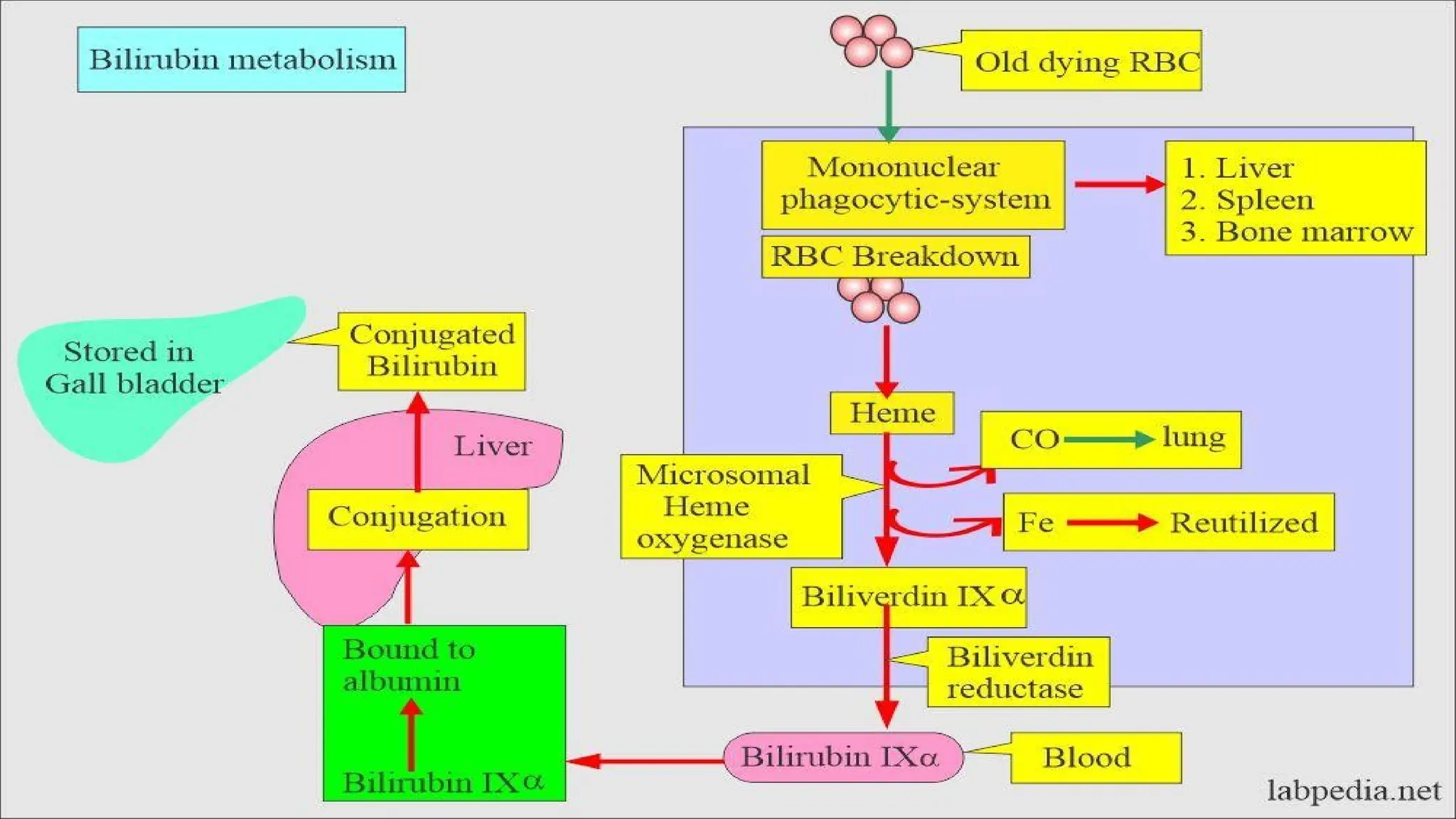
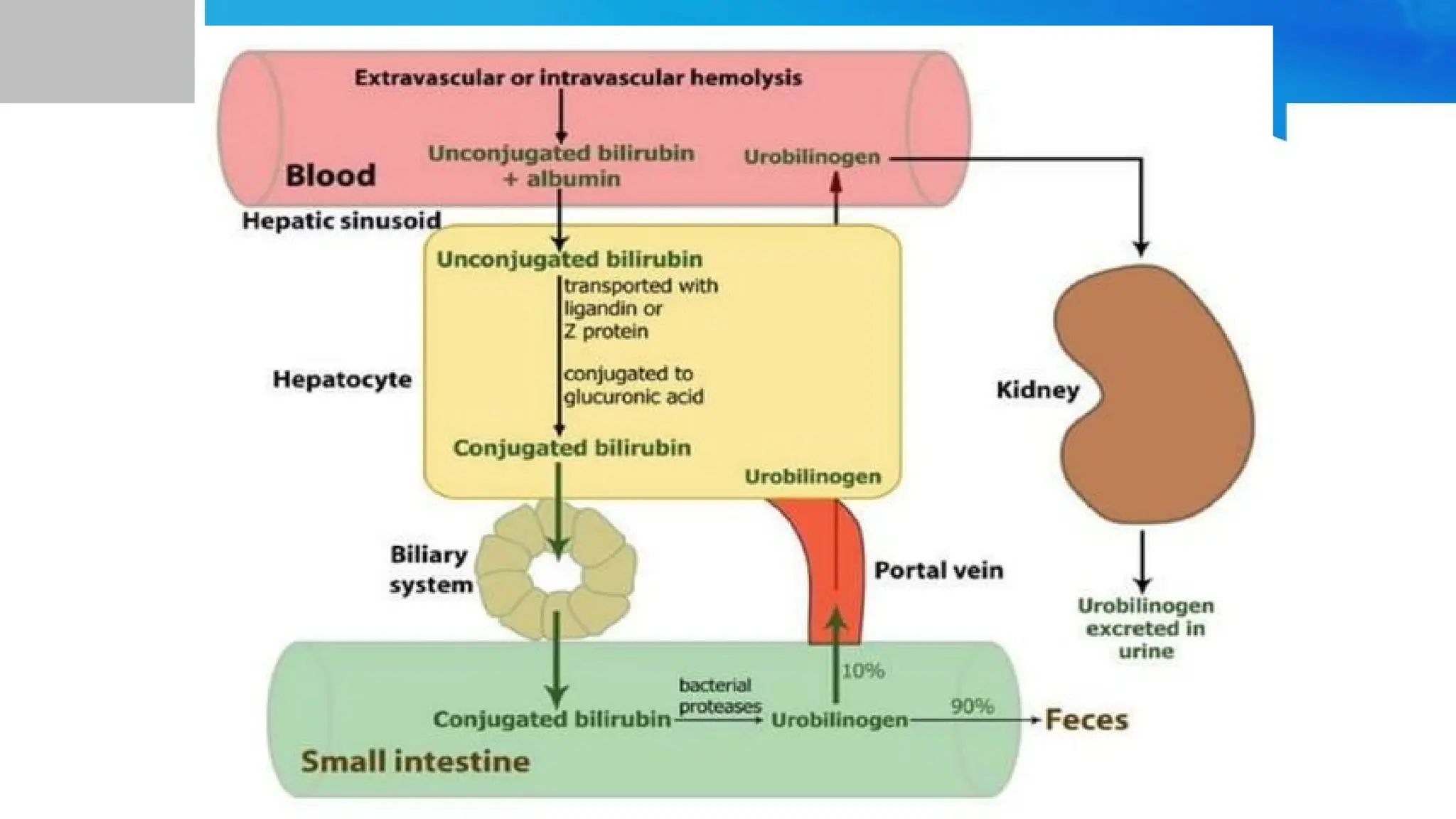
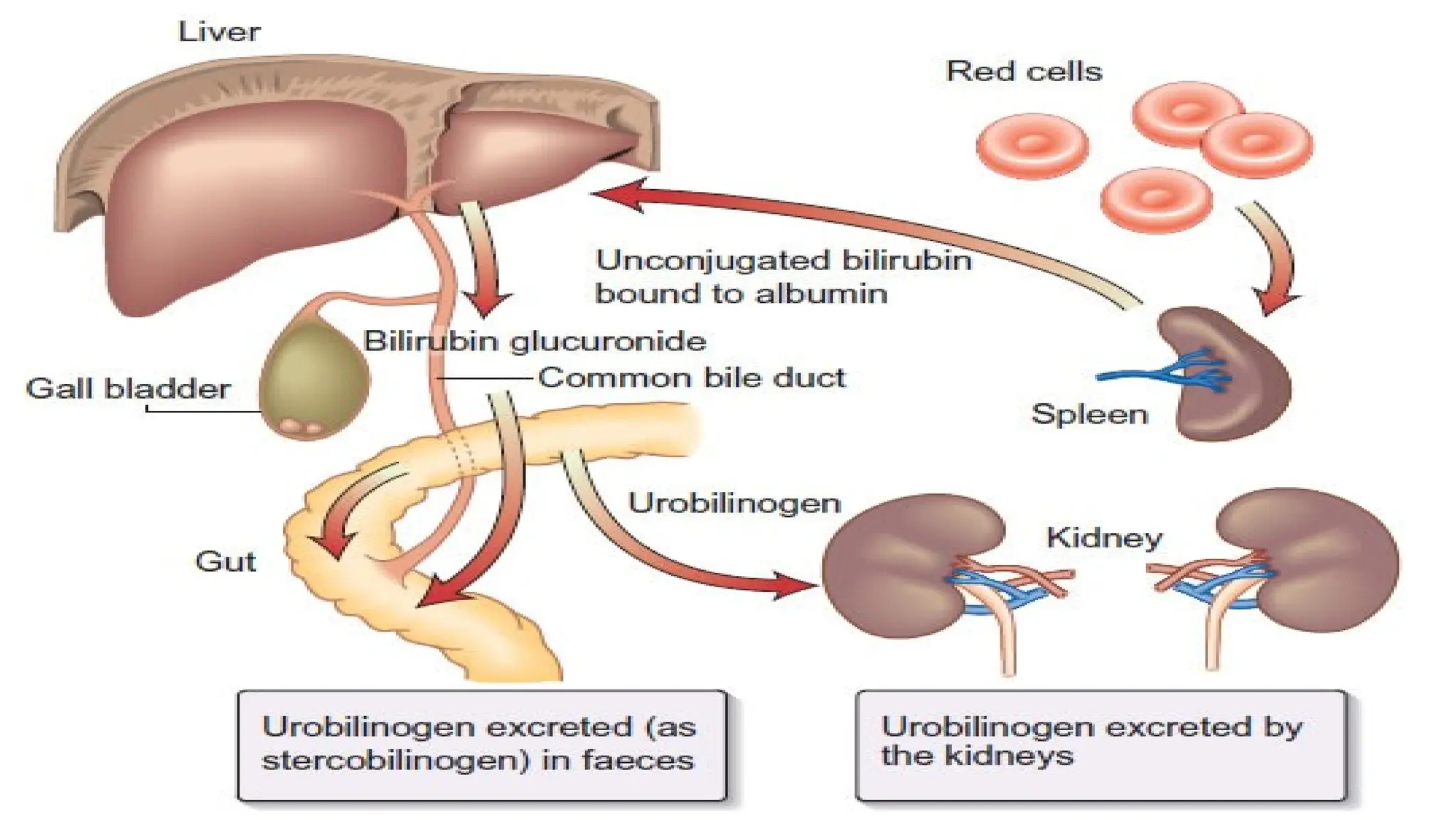
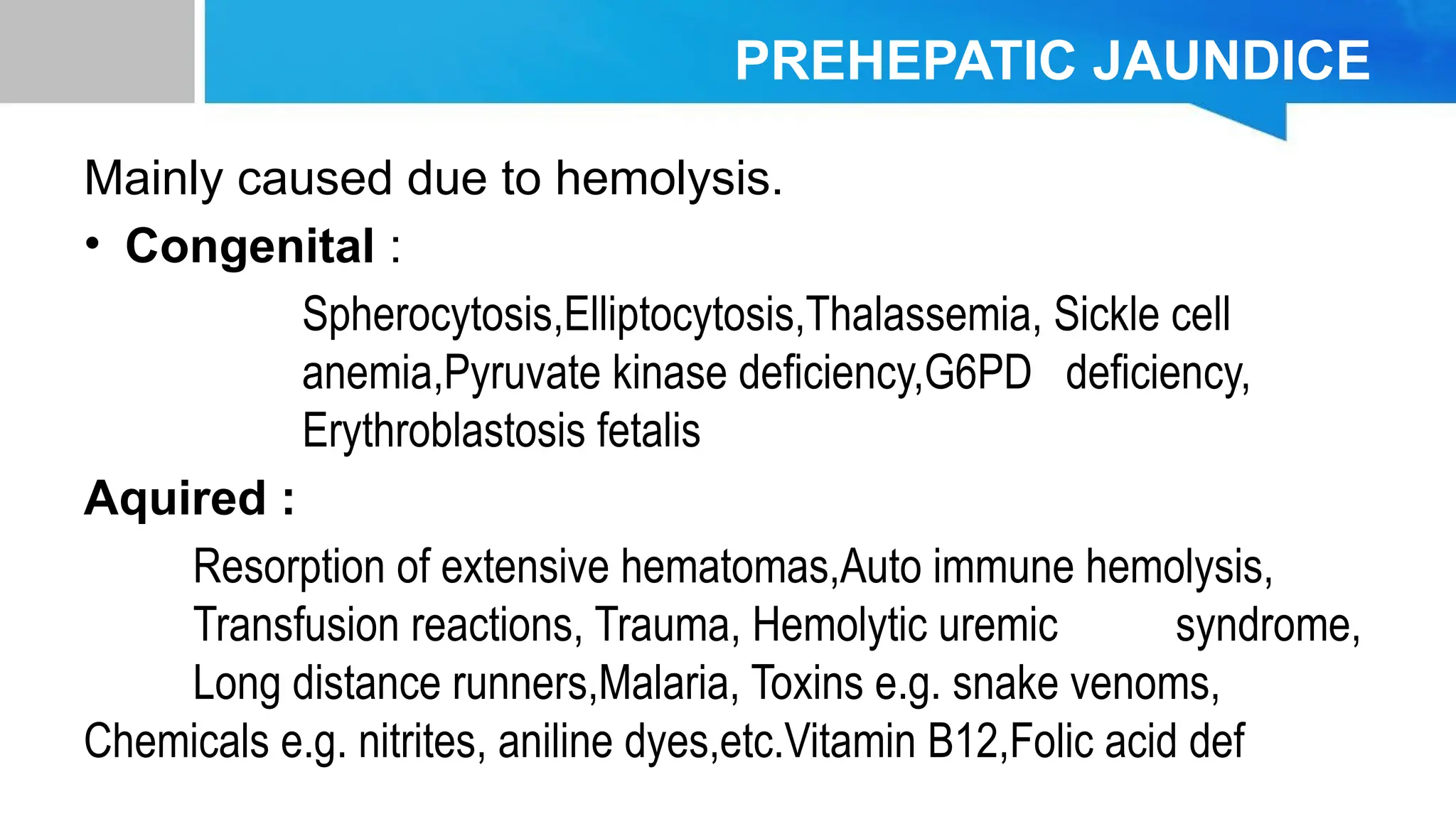
The document provides an overview of bilirubin metabolism and the different types of jaundice, which is characterized by the yellowing of skin and mucous membranes due to elevated bilirubin levels. Jaundice can be classified into pre-hepatic, hepatic, and post-hepatic based on the underlying causes, with specific conditions and symptoms associated with each type. It also explains the roles of various enzymes and pathologies in bilirubin processing and the implications of hyperbilirubinemia on health.