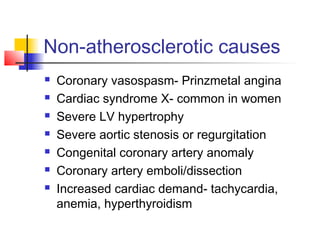
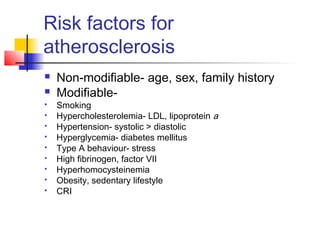
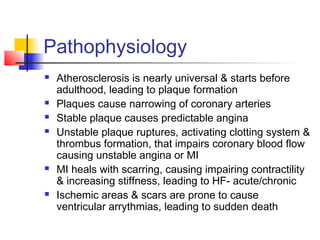
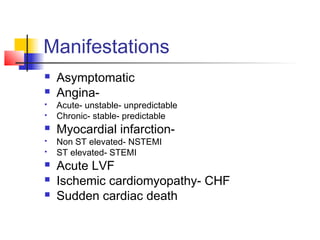
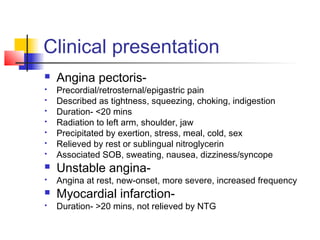
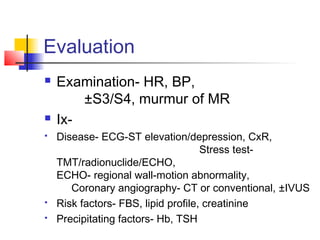
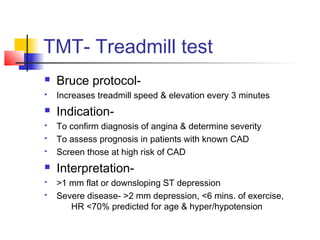
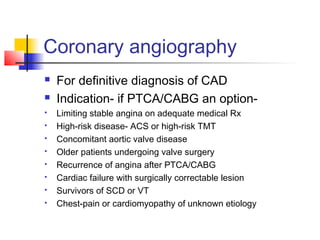
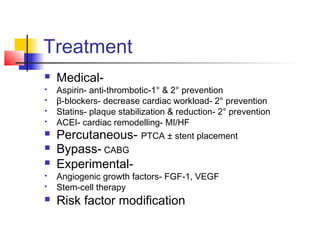
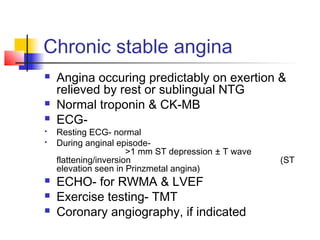
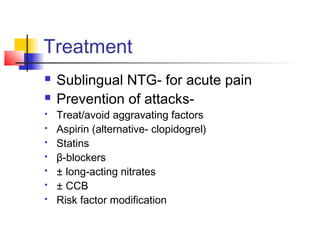
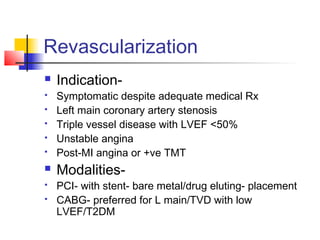
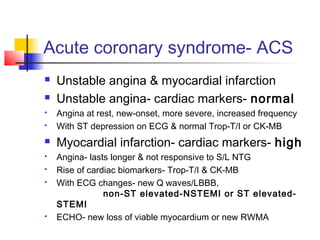
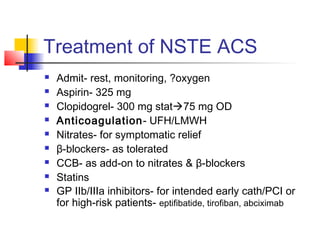
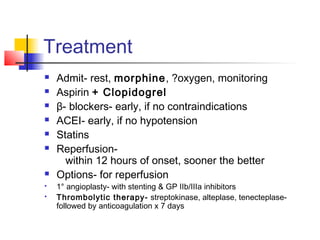
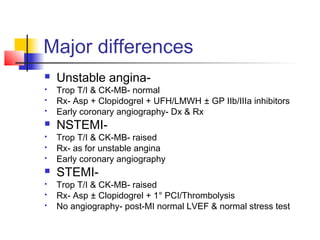
Coronary heart disease is caused by inadequate blood flow to the heart muscle due to atherosclerotic plaques narrowing the coronary arteries or other non-atherosclerotic causes. The most common cause is coronary artery disease (CAD) due to plaque accumulation over time from risk factors like smoking, hypertension, diabetes, and hypercholesterolemia. Clinical manifestations range from stable angina to heart attack. Diagnosis involves ECG, cardiac enzymes, stress testing, and coronary angiography. Treatment depends on severity and includes medical management, percutaneous interventions, bypass surgery, and risk factor modification.